Cardiovascular health is a topic of paramount importance, given the rising incidence of heart-related diseases globally.
Among the many conditions affecting the heart, arrhythmias and blood clots are particularly significant due to their potential severity and impact on overall health. This article explores the relationship between blood clots and arrhythmias, examining whether and how blood clots can cause irregular heartbeats.
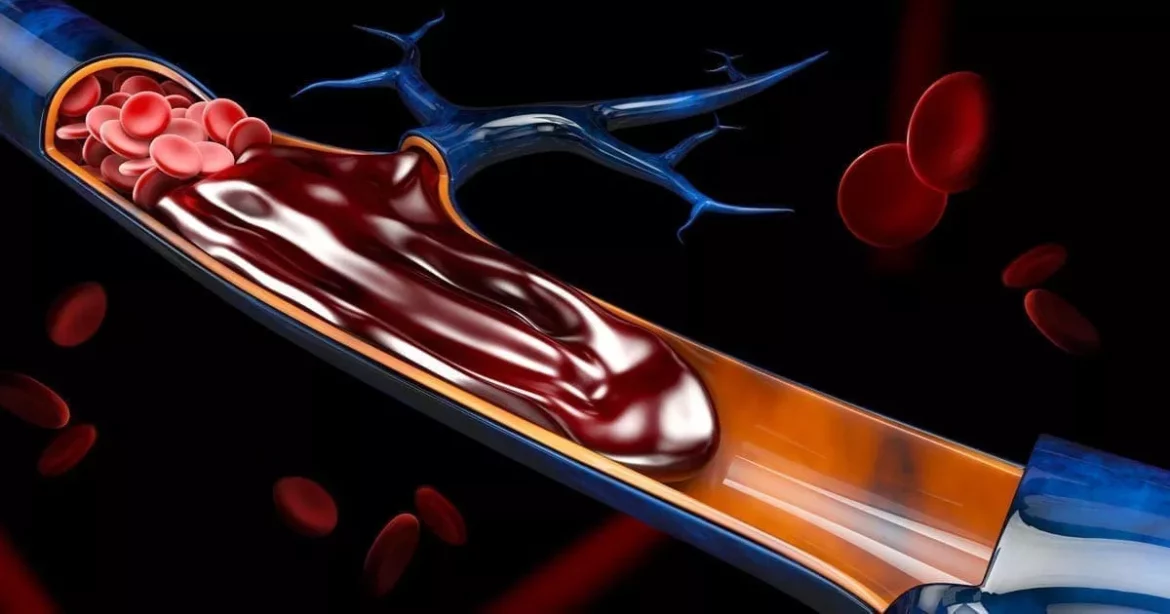
What Are Blood Clots?
Blood clots are gel-like collections of blood that form in veins or arteries. They are part of the body’s natural defense mechanism to prevent excessive bleeding when an injury occurs. However, when blood clots form inappropriately within blood vessels, they can pose significant health risks.
Types of Blood Clots
Thrombus: A clot that forms in a vein or artery.
Embolus: A clot that travels from one part of the body to another.
Deep Vein Thrombosis (DVT): A clot in a deep vein, usually in the legs.
Pulmonary Embolism (PE): A clot that travels to the lungs.
Atrial Thrombosis: A clot in the atrium of the heart.
See Also: can salt cause arrhythmia
Causes of Blood Clots
Inactivity or Immobilization: Prolonged periods of inactivity can slow blood flow and lead to clot formation.
Injury or Surgery: Trauma or surgical procedures can damage blood vessels, prompting clotting.
Medical Conditions: Conditions such as atrial fibrillation, obesity, and certain cancers increase clotting risk.
Lifestyle Factors: Smoking, dehydration, and certain medications can elevate clotting risk.
Causes of Arrhythmias
Heart Disease: Conditions like coronary artery disease or heart attack can damage the heart’s electrical system.
Electrolyte Imbalance: Abnormal levels of potassium, sodium, calcium, or magnesium can trigger arrhythmias.
Medication: Certain drugs, including those used to treat heart conditions, can cause arrhythmias as a side effect.
Can Blood Clots Cause Arrhythmias?
Mechanisms Linking Blood Clots to Arrhythmias
The relationship between blood clots and arrhythmias is complex and multifaceted. Blood clots can lead to arrhythmias through several mechanisms:
Atrial Fibrillation and Thrombus Formation: Atrial fibrillation can cause blood to pool in the atria, leading to clot formation. These clots can travel and cause strokes or other complications. Conversely, clots in the atria can exacerbate AFib by disrupting normal blood flow and increasing atrial pressure.
Pulmonary Embolism and Right Heart Strain: Pulmonary embolism can increase pressure in the right ventricle, leading to right ventricular strain and subsequent arrhythmias. The increased workload on the heart can disrupt the normal rhythm and lead to conditions such as atrial flutter or ventricular tachycardia.
Coronary Thrombosis and Ventricular Arrhythmias: Blood clots in the coronary arteries can lead to heart attacks, which can damage the heart muscle and its electrical pathways. This damage can cause ventricular arrhythmias, which are often severe and life-threatening.
Paradoxical Embolism: In cases of a patent foramen ovale (PFO), a blood clot can travel from the right side of the heart to the left side and enter systemic circulation. If it reaches the coronary arteries, it can cause a heart attack, leading to arrhythmias.
Clinical Evidence and Case Studies
Several studies and clinical observations support the link between blood clots and arrhythmias:
Study on AFib and Stroke: Research has shown that patients with AFib have a higher risk of stroke due to thrombus formation in the atria. The stroke risk increases with the presence of blood clots in the left atrium, highlighting the bidirectional relationship between AFib and thrombosis.
Case Study on PE and Arrhythmias: A study reported that patients with massive pulmonary embolism frequently develop arrhythmias, particularly right ventricular strain-related atrial flutter and ventricular tachycardia. The mechanical strain on the heart from PE is a significant trigger for these arrhythmias.
Heart Attack and Ventricular Arrhythmias: Clinical evidence indicates that patients who suffer from myocardial infarction due to coronary thrombosis are at high risk for developing ventricular arrhythmias. This underscores the role of blood clots in initiating life-threatening heart rhythm disturbances.
Prevention And Management
Preventing Blood Clots
Anticoagulation Therapy: Medications like warfarin, heparin, and newer anticoagulants (e.g., rivaroxaban, apixaban) are commonly used to prevent clot formation, especially in high-risk individuals.
Lifestyle Modifications: Regular physical activity, maintaining a healthy weight, staying hydrated, and avoiding smoking can reduce the risk of clot formation.
Medical Interventions: For individuals with a high risk of clots, medical devices such as inferior vena cava (IVC) filters can be used to prevent clots from traveling to the lungs.
Managing Arrhythmias
Medication: Antiarrhythmic drugs can help control heart rhythm. Beta-blockers, calcium channel blockers, and other medications can stabilize the heart’s electrical activity.
Procedures: In severe cases, procedures such as catheter ablation, pacemaker implantation, or cardioversion may be necessary to restore normal heart rhythm.
Monitoring and Follow-up: Regular monitoring of heart rhythm and clotting status is crucial for individuals with a history of arrhythmias or blood clots. This can help detect and manage complications early.
Conclusion
The interplay between blood clots and arrhythmias is a critical aspect of cardiovascular health. Blood clots can indeed cause arrhythmias through various mechanisms, including atrial fibrillation, pulmonary embolism, and coronary thrombosis.
Understanding this relationship is essential for preventing and managing these conditions effectively. Through appropriate medical interventions, lifestyle modifications, and vigilant monitoring, the risks associated with blood clots and arrhythmias can be significantly reduced, improving overall heart health and patient outcomes.