Severe aortic stenosis is a serious heart condition characterized by the narrowing of the aortic valve opening, which obstructs blood flow from the left ventricle to the aorta and subsequently to the rest of the body.
This condition can lead to significant health issues, including heart failure, arrhythmias, and even sudden cardiac death.
Understanding the life expectancy of individuals with severe aortic stenosis is crucial for patients, families, and healthcare providers in order to make informed decisions about treatment and management.
Understanding Aortic Stenosis
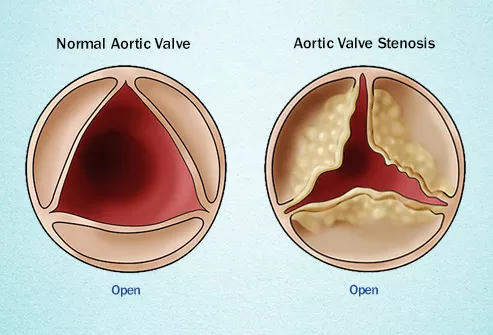
Aortic stenosis occurs when the aortic valve, which regulates blood flow from the heart into the aorta, becomes narrowed and restricts blood flow. This condition can develop due to congenital heart defects, rheumatic fever, or the accumulation of calcium deposits on the valve. As the valve narrows, the heart must work harder to pump blood through the reduced opening, leading to increased pressure within the heart and potentially causing damage to the heart muscle over time.
Symptoms of Severe Aortic Stenosis
Patients with severe aortic stenosis may experience a range of symptoms, including:
- Chest pain or angina
- Shortness of breath, especially during exertion
- Fatigue and weakness
- Dizziness or fainting (syncope)
- Palpitations or irregular heartbeats
These symptoms can significantly impact a patient’s quality of life and indicate the need for prompt medical attention.
See Also: Can Exercise Reverse Coronary Artery Disease
Diagnosis and Assessment
The diagnosis of aortic stenosis typically involves a combination of medical history, physical examination, and diagnostic tests such as echocardiography, which uses ultrasound to visualize the heart and measure the severity of the valve narrowing. Additional tests, such as electrocardiograms (ECGs), chest X-rays, and cardiac catheterization, may also be used to assess the extent of the condition and plan appropriate treatment strategies.
Treatment Options
Treatment for severe aortic stenosis depends on the severity of the condition, the presence of symptoms, and the patient’s overall health. The primary treatment options include:
Medications: While medications cannot cure aortic stenosis, they can help manage symptoms and improve heart function.
Commonly prescribed medications include beta-blockers, ACE inhibitors, and diuretics.
Surgical Aortic Valve Replacement (SAVR): This traditional open-heart surgery involves removing the damaged aortic valve and replacing it with a mechanical or biological valve. SAVR is considered the gold standard treatment for severe aortic stenosis and can significantly improve survival rates and quality of life.
Transcatheter Aortic Valve Replacement (TAVR): TAVR is a less invasive procedure in which a new valve is implanted via a catheter inserted through the femoral artery or another access point. TAVR is often recommended for patients who are at high or intermediate risk for open-heart surgery.
Prognosis And Life Expe ctancy
The prognosis for individuals with severe aortic stenosis varies based on several factors, including the severity of the condition, the presence of symptoms, and the patient’s overall health. Without treatment, severe aortic stenosis has a poor prognosis, with an average survival rate of 2 to 3 years after the onset of symptoms. However, with appropriate treatment, the outlook improves significantly.
Factors Affecting Life Expectancy
Several factors can influence the life expectancy of individuals with severe aortic stenosis:
Timely Intervention: Early diagnosis and timely intervention, such as valve replacement surgery, are critical in improving survival rates and quality of life.
Age and Overall Health: Younger patients and those with fewer comorbidities tend to have better outcomes following treatment.
Severity of Symptoms: Patients with severe symptoms at the time of diagnosis may have a poorer prognosis compared to those with mild or no symptoms.
Heart Function: The overall function of the heart, including the presence of heart failure or other cardiovascular conditions, can impact life expectancy.
Impact of Treatment on Survival Rates
Surgical aortic valve replacement (SAVR) and transcatheter aortic valve replacement (TAVR) have been shown to significantly improve survival rates for patients with severe aortic stenosis. Studies indicate that patients who undergo SAVR have a 5-year survival rate of approximately 80%, while those who undergo TAVR have a comparable survival rate, particularly in high-risk patient populations.
Quality of Life Post-Treatment
In addition to improving survival rates, valve replacement procedures can greatly enhance the quality of life for patients with severe aortic stenosis. Many patients report significant improvements in symptoms, including reduced chest pain, increased exercise tolerance, and improved overall well-being. Regular follow-up care and lifestyle modifications, such as maintaining a healthy diet, engaging in regular physical activity, and managing other health conditions, are essential for optimizing outcomes and maintaining heart health.
Living with Severe Aortic Stenosis
For patients living with severe aortic stenosis, managing the condition involves regular monitoring, adhering to prescribed treatments, and making lifestyle changes to support heart health. It is important for patients to:
Follow Medical Advice: Adhere to prescribed medications and attend regular follow-up appointments with healthcare providers.
Adopt a Heart-Healthy Lifestyle: Maintain a balanced diet, engage in regular physical activity, avoid smoking, and limit alcohol consumption.
Monitor Symptoms: Be vigilant about any changes in symptoms and seek prompt medical attention if new or worsening symptoms occur.
Conclusion
Severe aortic stenosis is a serious condition that requires prompt medical attention and appropriate treatment to improve survival rates and quality of life. With advances in surgical and minimally invasive procedures, many patients with severe aortic stenosis can achieve significant improvements in their prognosis and overall well-being. Early diagnosis, timely intervention, and a commitment to heart-healthy lifestyle changes are key factors in managing this condition and ensuring the best possible outcomes for patients.