Vasospastic angina is a condition characterized by sudden, intense chest pain due to transient spasms in the coronary arteries. Unlike stable angina, which is usually triggered by physical exertion or stress, vasospastic angina can occur at rest, often in the early morning hours. These spasms reduce or temporarily stop blood flow to part of the heart muscle, leading to ischemic pain. Understanding the causes and mechanisms of this condition is essential for developing effective treatment strategies and improving patient outcomes.
Understanding Vasospastic Angina
Vasospastic angina was first described by Dr. Myron Prinzmetal in 1959. It is a less common form of angina but can be just as serious as other types. The hallmark of vasospastic angina is the occurrence of chest pain due to spasms in the coronary arteries, which can occur without any underlying coronary artery disease. These spasms can vary in duration and intensity, leading to unpredictable and often severe chest pain episodes.
Pathophysiology of Vasospastic Angina
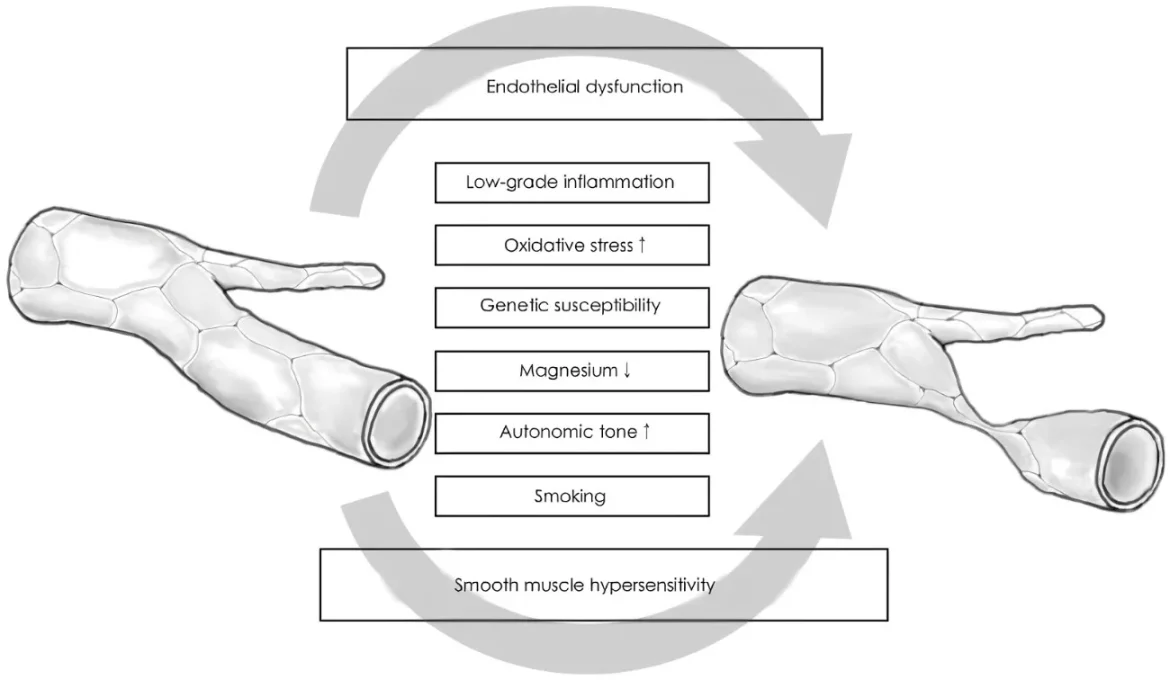
The exact mechanisms that cause vasospastic angina are not fully understood, but it is believed to involve several factors, including endothelial dysfunction, increased smooth muscle reactivity, and autonomic nervous system imbalances.
Endothelial Dysfunction
The endothelium is the inner lining of blood vessels and plays a crucial role in maintaining vascular health. It produces substances that help regulate blood vessel tone, blood clotting, and immune function. In vasospastic angina, endothelial dysfunction is thought to play a significant role. When the endothelium is damaged or does not function properly, it can lead to an imbalance between vasodilatory and vasoconstrictive substances. This imbalance can cause the coronary arteries to spasm.
See Also: how long can a person live with severe aortic stenosis
Increased Smooth Muscle Reactivity
Smooth muscle cells in the walls of coronary arteries are responsible for contracting and relaxing to regulate blood flow. In individuals with vasospastic angina, these smooth muscle cells may be overly reactive, leading to spontaneous and exaggerated contractions. Factors such as inflammation, oxidative stress, and genetic predisposition can contribute to this increased reactivity.
Autonomic Nervous System Imbalances
The autonomic nervous system, which controls involuntary bodily functions, including heart rate and blood vessel tone, may also play a role in vasospastic angina. An imbalance between the sympathetic (fight or flight) and parasympathetic (rest and digest) branches of the autonomic nervous system can influence coronary artery tone and contribute to spasms.
Causes and Risk Factors
Several factors can trigger or exacerbate the spasms associated with vasospastic angina. These include:
Smoking
Smoking is a significant risk factor for vasospastic angina. Nicotine and other chemicals in tobacco smoke can damage the endothelium, increase oxidative stress, and promote inflammation, all of which can contribute to coronary artery spasms.
Cold Exposure
Exposure to cold temperatures can cause blood vessels to constrict, potentially triggering spasms in individuals with vasospastic angina. This response is part of the body’s effort to preserve heat but can inadvertently reduce blood flow to the heart.
Medications
Certain medications, particularly those that affect blood vessel tone, can induce or exacerbate vasospastic angina. These include medications like ergotamine (used for migraines), amphetamines, and some chemotherapy drugs.
Substance Use
Illicit drugs such as cocaine can cause intense coronary artery spasms and are a known risk factor for vasospastic angina. Cocaine stimulates the sympathetic nervous system, leading to vasoconstriction and increased myocardial oxygen demand.
Emotional Stress
Emotional stress can activate the sympathetic nervous system, leading to increased heart rate and blood pressure, which can precipitate coronary artery spasms. Managing stress is important for individuals prone to vasospastic angina.
Other Medical Conditions
Other conditions, such as migraines, Raynaud’s phenomenon, and certain autoimmune disorders, have been associated with an increased risk of vasospastic angina. These conditions can involve similar mechanisms of vascular dysfunction and hyperreactivity.
Symptoms And Diagnosis
The symptoms of vasospastic angina can mimic those of other forms of angina or heart conditions, making diagnosis challenging. Key symptoms include:
- Sudden chest pain, often occurring at rest
- Pain that may radiate to the arms, shoulders, neck, or jaw
- Episodes that typically occur early in the morning or during sleep
- Pain lasting from a few minutes to half an hour
Diagnosis involves a combination of patient history, physical examination, and diagnostic tests. These may include:
Electrocardiogram (ECG)
During an angina episode, an ECG can show transient ST-segment elevation, indicating myocardial ischemia. However, a normal ECG between episodes does not rule out vasospastic angina.
Ambulatory ECG Monitoring
Holter monitoring or event recorders can capture ECG changes during daily activities and help diagnose intermittent episodes of vasospastic angina.
Coronary Angiography
This imaging technique visualizes the coronary arteries and can help identify spasms. Provocative testing with agents like acetylcholine or ergonovine may be used during angiography to induce and observe spasms.
Blood Tests
Blood tests can help rule out other conditions and assess for markers of inflammation or other abnormalities that may contribute to coronary artery spasms.
Treatment and Management
Treatment for vasospastic angina aims to prevent spasms, relieve symptoms, and reduce the risk of complications. Key components of treatment include:
Lifestyle Modifications
Smoking Cessation: Quitting smoking is crucial as it can significantly reduce the frequency and severity of spasms.
Stress Management: Techniques such as meditation, yoga, and counseling can elp manage stress and reduce the risk of angina episodes.
Avoiding Triggers: Identifying and avoiding known triggers, such as cold exposure and certain medications, is important.
Medications
Calcium Channel Blockers: These medications, such as diltiazem and amlodipine, are first-line treatments for vasospastic angina. They help relax the coronary arteries and prevent spasms.
Nitrates: Long-acting nitrates can also help prevent spasms and relieve chest pain.
Statins: While primarily used to lower cholesterol, statins may also have beneficial effects on endothelial function and reduce the risk of spasms.
Antiplatelet Agents: Low-dose aspirin or other antiplatelet agents may be used to prevent blood clots that could exacerbate spasms.
Interventional Procedures
In severe cases where medical management is insufficient, interventional procedures such as percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG) may be considered.
Preventive Measures
Preventing vasospastic angina involves managing risk factors and adhering to treatment plans. Key preventive measures include:
Regular Follow-Up: Regular visits to a healthcare provider to monitor and adjust treatment as needed.
Healthy Lifestyle: Maintaining a healthy diet, regular exercise, and avoiding smoking and excessive alcohol consumption.
Medication Adherence: Taking prescribed medications as directed to control symptoms and prevent episodes.
Conclusion
Vasospastic angina is a condition that requires careful management to prevent serious complications such as heart attacks.
Understanding the causes and risk factors is essential for effective treatment and prevention. By addressing lifestyle factors, adhering to medical treatment, and managing stress, individuals with vasospastic angina can lead healthier lives and reduce the frequency and severity of angina episodes. Continued research into the underlying mechanisms of coronary artery spasms will further enhance our ability to treat and prevent this condition.