Right heart failure, also known as right ventricular failure, is a condition where the right side of the heart loses its ability to pump blood efficiently. This dysfunction leads to a backlog of blood in the veins and a reduced flow of blood to the lungs.
Right heart failure is often a consequence of underlying heart conditions, and identifying the most common causes is crucial for effective diagnosis and treatment. This article explores the primary cause of right heart failure, its pathophysiology, and the associated risk factors, symptoms, and treatment options.
Most Common Cause of Right Heart Failure: Left-Sided Heart Failure
Left-Sided Heart Failure as the Primary Cause
Left-sided heart failure is the most common cause of right heart failure. In left-sided heart failure, the left ventricle cannot effectively pump blood to the systemic circulation, leading to increased pressure in the left atrium and pulmonary veins.
This elevated pressure is transmitted backward into the pulmonary circulation, resulting in increased pulmonary artery pressure and resistance. The right ventricle, which is responsible for pumping blood into the lungs, must work harder to overcome this increased resistance. Over time, the right ventricle may become weakened and dilated, eventually leading to right heart failure.
See Also: What Causes Congestive Heart
Pathophysiology of Right Heart Failure Due to Left-Sided Heart Failure
The pathophysiological process linking left-sided heart failure to right heart failure involves several key mechanisms:
Increased Pulmonary Pressure: Left-sided heart failure causes an increase in pulmonary venous pressure, which is transmitted to the pulmonary arteries. This condition is known as pulmonary hypertension, and it forces the right ventricle to work harder to pump blood into the lungs.
Right Ventricular Overload: The right ventricle, facing increased afterload due to pulmonary hypertension, undergoes hypertrophy (thickening of the ventricular wall) to maintain cardiac output. Over time, this compensatory mechanism becomes inadequate, leading to right ventricular dilation and dysfunction.
Reduced Right Ventricular Output: As the right ventricle fails, it cannot pump sufficient blood to the lungs, leading to reduced oxygenation and a decrease in overall cardiac output. This results in systemic venous congestion, manifesting as symptoms of right heart failure.
Other Contributing Factors And Causes
While left-sided heart failure is the most common cause of right heart failure, several other conditions can contribute to or independently cause right heart failure:
Pulmonary Hypertension
Pulmonary hypertension, defined as elevated pressure in the pulmonary arteries, is a significant contributor to right heart failure. It can result from chronic lung diseases such as chronic obstructive pulmonary disease (COPD), interstitial lung disease, or pulmonary embolism. Pulmonary arterial hypertension (PAH), a rare but severe condition, involves increased pressure in the pulmonary arteries without left heart disease and can lead to right ventricular failure.
CorPulmonale
Corpulmonale refers to right ventricular enlargement and failure due to lung disease or pulmonary hypertension. Chronic hypoxemia (low oxygen levels) in conditions such as COPD or sleep apnea leads to pulmonary vasoconstriction, increasing pulmonary artery pressure and straining the right ventricle.
see also: How Do Doctors Test for Congestive Heart Failure
Congenital Heart Disease
Certain congenital heart defects, such as atrial septal defects, ventricular septal defects, and Eisenmenger syndrome, can cause right heart failure. These defects result in abnormal blood flow patterns that overload the right ventricle over time.
Myocardial Infarction
A myocardial infarction (heart attack) involving the right ventricle, although less common than left ventricular infarction, can directly damage the right ventricle and lead to right heart failure. This condition, known as right ventricular infarction, often occurs in conjunction with inferior wall myocardial infarction.
Cardiomyopathy
Cardiomyopathies, such as dilated cardiomyopathy, hypertrophic cardiomyopathy, and restrictive cardiomyopathy, can affect both sides of the heart. When the right ventricle is predominantly involved, it can lead to right heart failure.
Risk Factors for Right Heart Failure
Several risk factors increasec the likelihood of developing right heart failure, especially when combined with the conditions mentioned above:
Age: The risk of heart failure increases with age, as the heart’s pumping ability naturally declines.
Hypertension: Chronic high blood pressure can lead to left-sided heart failure, subsequently causing right heart failure.
Coronary Artery Disease: Blocked or narrowed coronary arteries reduce blood supply to the heart muscle, leading to myocardial infarction and heart failure.
Diabetes: Diabetes increases the risk of coronary artery disease and hypertension, contributing to heart failure.
Obesity: Excess body weight strains the heart and increases the risk of developing heart failure.
Smoking: Smoking damages blood vessels and increases the risk of coronary artery disease and lung diseases, leading to heart failure.
Chronic Lung Diseases: Conditions like COPD and interstitial lung disease increase the risk of pulmonary hypertension and right heart failure.
Symptoms of Right Heart Failure
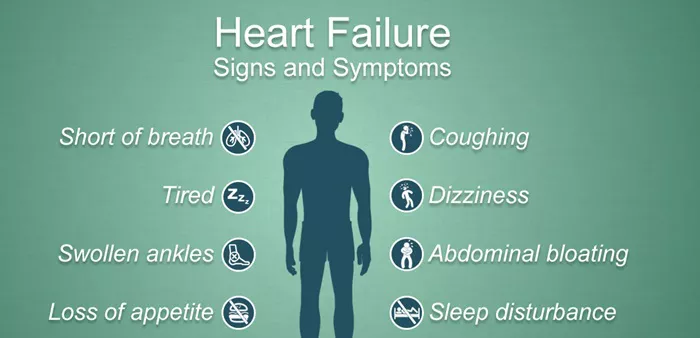
Right heart failure manifests through a range of symptoms related to systemic venous congestion and reduced cardiac output. Common symptoms include:
Edema: Swelling in the legs, ankles, and feet due to fluid retention.
Ascites: Accumulation of fluid in the abdominal cavity, causing abdominal swelling and discomfort.
Jugular Venous Distension: Visible bulging of the jugular veins in the neck due to increased venous pressure.
Hepatomegaly: Enlarged liver caused by congestion of blood flow in the hepatic veins.
Fatigue: Reduced cardiac output leads to decreased oxygen delivery to tissues, resulting in fatigue and weakness.
Shortness of Breath: Fluid buildup in the lungs (pulmonary congestion) can cause difficulty breathing, particularly during exertion or when lying flat.
Diagnosis of Right Heart Failure
Diagnosing right heart failure involves a comprehensive clinical evaluation, including a detailed medical history, physical examination, and diagnostic tests. Key diagnostic tools include:
Echocardiography: An ultrasound of the heart that provides detailed images of heart structures and assesses right ventricular function and pulmonary pressures.
Electrocardiogram (ECG): Records the electrical activity of the heart and can reveal signs of right ventricular strain or hypertrophy.
Chest X-ray: Provides images of the heart and lungs, revealing signs of pulmonary congestion and right ventricular enlargement.
Cardiac MRI: Offers detailed images of heart structures and function, helping to assess right ventricular size and function.
Blood Tests: Measure biomarkers such as B-type natriuretic peptide (BNP) or N-terminal pro-BNP (NT-proBNP), which are elevated in heart failure.
Right Heart Catheterization: Invasive procedure that measures pressures within the right side of the heart and pulmonary arteries, providing definitive diagnosis of pulmonary hypertension.
Treatment of Right Heart Failure
Treatment of right heart failure focuses on managing the underlying cause, alleviating symptoms, and improving quality of life. Common treatment strategies include:
Medications: Diuretics help reduce fluid buildup, while vasodilators lower pulmonary artery pressure. Beta-blockers and ACE inhibitors may be used to manage heart failure symptoms and improve heart function.
Oxygen Therapy: Supplemental oxygen can help relieve symptoms in patients with hypoxemia.
Lifestyle Modifications: Dietary changes, weight management, smoking cessation, and regular exercise can improve overall heart health and reduce symptoms.
Management of Underlying Conditions: Treating conditions such as left-sided heart failure, pulmonary hypertension, and lung diseases is crucial for preventing progression to right heart failure.
Surgical Interventions: In severe cases, surgical procedures such as heart valve repair or replacement, implantation of a ventricular assist device (VAD), or heart transplantation may be necessary.
Conclusion
Right heart failure is a complex condition often secondary to left-sided heart failure, making it the most common cause.
Understanding the interplay between left and right heart function is essential for accurate diagnosis and effective treatment. Managing risk factors, treating underlying conditions, and adopting a heart-healthy lifestyle can significantly improve outcomes for individuals with right heart failure.
By addressing the root causes and providing comprehensive care, healthcare providers can help patients manage their symptoms and enhance their quality of life.