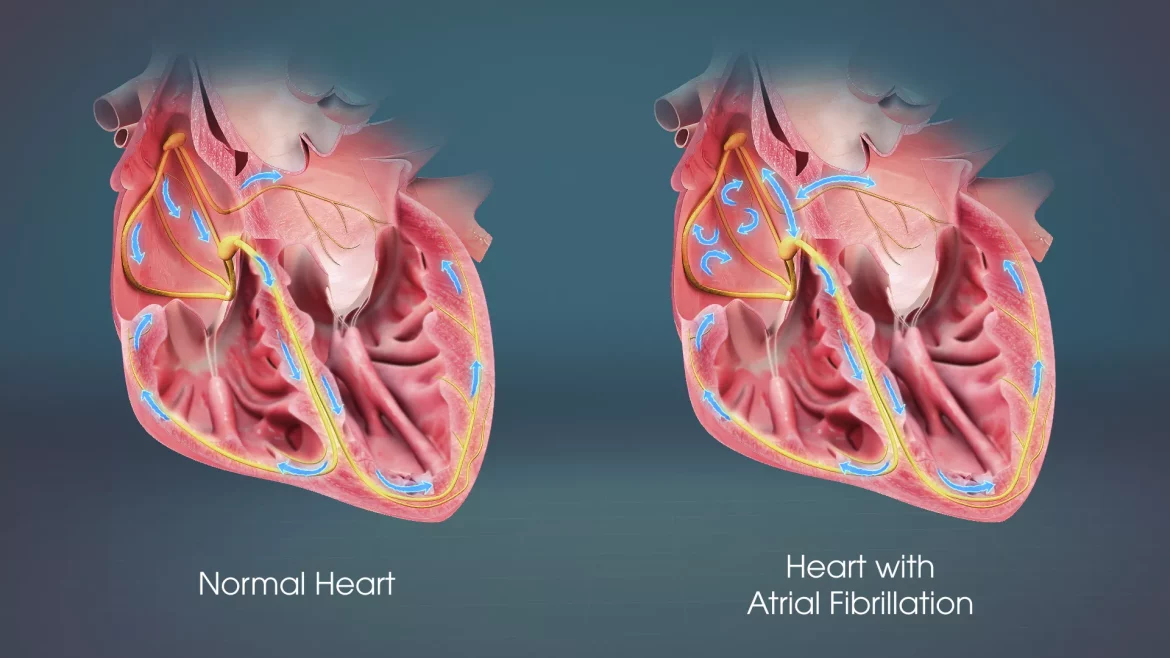
Atrial fibrillation, often abbreviated as AFib or AF, is a common type of arrhythmia, which is a problem with the rate or rhythm of the heartbeat.
It occurs when the heart’s two upper chambers (the atria) beat irregularly and out of sync with the two lower chambers (the ventricles). This can lead to poor blood flow and a variety of symptoms, ranging from mild to severe.
Understanding when atrial fibrillation occurs can help in managing and preventing this condition. This article delves into the various triggers, risk factors, and underlying conditions that can lead to the onset of atrial fibrillation.
There are different types of atrial fibrillation, including:
Paroxysmal AFib: Episodes come and go, usually stopping on their own within a few hours or days.
Persistent AFib: Episodes last longer than seven days and may require treatment to restore normal rhythm.
Permanent AFib: The irregular heart rhythm can’t be restored, and treatment focuses on managing symptoms.
When Does Atrial Fibrillation Occur?
Triggers and Risk Factors
Several factors can trigger atrial fibrillation or increase the risk of developing this arrhythmia. Understanding these triggers is crucial for both prevention and management.
1. Age
Atrial fibrillation becomes more common with age. The risk of developing AFib increases significantly in individuals over the age of 65. This is likely due to age-related changes in the heart and its electrical system.
see also: What Will The Er Do for Afib?
2. Heart Conditions
Various heart-related conditions can increase the risk of atrial fibrillation:
High Blood Pressure (Hypertension): Chronic high blood pressure can cause changes in the heart’s structure, such as thickening of the heart muscle, which can trigger AFib.
Heart Attack: Damage to the heart tissue from a heart attack can disrupt normal electrical signals, leading to atrial fibrillation.
Heart Valve Problems: Issues with the heart valves, especially the mitral valve, can contribute to AFib.
Congestive Heart Failure: This condition weakens the heart’s ability to pump blood efficiently, increasing the risk of atrial fibrillation.
3. Lifestyle Factors
Certain lifestyle factors can also trigger atrial fibrillation:
Alcohol Consumption: Excessive alcohol intake can lead to “holiday heart syndrome,” where binge drinking causes AFib.
Caffeine: High caffeine intake can act as a stimulant and trigger atrial fibrillation in some individuals.
Obesity: Being overweight can increase the risk of developing AFib due to added stress on the heart.
4. Other Medical Conditions
Other health conditions can contribute to the onset of atrial fibrillation:
Thyroid Problems: Both hyperthyroidism (overactive thyroid) and hypothyroidism (underactive thyroid) can affect heart rhythm.
Sleep Apnea: This condition, characterized by interrupted breathing during sleep, is associated with an increased risk of atrial fibrillation.
Diabetes: Having diabetes can increase the risk of AFib due to its impact on overall cardiovascular health.
5. Genetic Factors
Family history plays a role in the risk of developing atrial fibrillation. If a close relative has AFib, your chances of developing it are higher.
6. Acute Triggers
Certain acute events or conditions can temporarily trigger atrial fibrillation:
Infections: Severe infections, especially those causing high fever or affecting the heart or lungs, can trigger AFib.
Surgery: Especially heart surgery, can lead to temporary atrial fibrillation.
Stress: Both physical and emotional stress can trigger AFib episodes.
Symptoms And Diagnosis
Symptoms
Atrial fibrillation symptoms can vary greatly between individuals. Some people may have no symptoms at all, while others may experience:
- Palpitations (sensations of a racing, uncomfortable, or irregular heartbeat)
- Weakness
- Reduced ability to exercise
- Fatigue
- Lightheadedness or dizziness
- Shortness of breath
- Chest pain
Diagnosis
Diagnosing atrial fibrillation involves several steps:
Medical History and Physical Exam: The doctor will ask about your symptoms, medical history, and any family history of heart conditions. They will also perform a physical exam, checking for signs of atrial fibrillation.
Electrocardiogram (ECG or EKG): This is the primary test for diagnosing AFib. It records the electrical activity of your heart and can detect irregularities.
Holter Monitor: This portable ECG device is worn for 24 to 48 hours to record the heart’s activity over time.
Event Recorder: Similar to a Holter monitor, but used for longer periods (up to 30 days) to detect intermittent episodes of AFib.
Echocardiogram: This ultrasound of the heart can help identify underlying structural heart problems that may be causing atrial fibrillation.
Blood Tests: These can check for thyroid problems and other conditions that might trigger AFib.
Stress Test: This test involves exercising while your heart activity is monitored to see if physical activity triggers AFib.
Treatment And Management
Lifestyle Modifications
Making lifestyle changes can help manage atrial fibrillation and reduce the frequency of episodes:
Healthy Diet: Eating a balanced diet rich in fruits, vegetables, whole grains, and lean proteins can support heart health.
Regular Exercise: Physical activity helps maintain a healthy weight and reduces the risk of cardiovascular disease.
Limit Alcohol and Caffeine: Reducing consumption of these substances can help prevent AFib episodes.
Quit Smoking: Smoking is a significant risk factor for heart disease and atrial fibrillation.
Medications
Several types of medications can be used to treat atrial fibrillation:
Rate Control Medications: These help control the heart rate, such as beta-blockers and calcium channel blockers.
Rhythm Control Medications: Antiarrhythmic drugs can help maintain a normal heart rhythm.
Blood Thinners: Anticoagulants reduce the risk of stroke by preventing blood clots from forming.
Procedures
In some cases, medical procedures may be necessary to manage atrial fibrillation:
Electrical Cardioversion: This procedure uses a controlled electric shock to restore a normal heart rhythm.
Catheter Ablation: A minimally invasive procedure where a catheter is used to destroy the tissue causing the abnormal electrical signals.
Surgery: In severe cases, surgical options like the Maze procedure can create new pathways for electrical signals in the heart.
Prevention
Preventing atrial fibrillation involves managing risk factors and leading a heart-healthy lifestyle. This includes regular check-ups with your healthcare provider, especially if you have a family history of AFib or other risk factors. Monitoring and controlling conditions like hypertension, diabetes, and thyroid problems are also crucial.
Monitoring And Follow-Up
Regular monitoring and follow-up with a healthcare provider are essential for managing atrial fibrillation effectively. This includes:
Routine ECGs: Regular electrocardiograms to monitor heart rhythm.
Blood Tests: Regular blood tests to check for conditions that can affect heart health.
Holter or Event Monitors: As needed, to track heart activity over time.
Living with Atrial Fibrillation
Living with atrial fibrillation requires ongoing management and lifestyle adjustments. It’s essential to:
Take Medications as Prescribed: Follow your doctor’s instructions regarding medication.
Regular Exercise: Maintain a routine that includes physical activity, but consult your doctor about safe levels of exercise.
Healthy Diet: Eat a balanced diet that supports heart health.
Avoid Triggers: Identify and avoid specific triggers that cause AFib episodes.
Stay Informed: Keep up with the latest information and treatments for atrial fibrillation.
Conclusion
Atrial fibrillation is a common but serious condition that requires careful management. Understanding when atrial fibrillation occurs, recognizing the triggers and risk factors, and knowing the symptoms can help in early detection and effective treatment. By making lifestyle changes, taking medications as prescribed, and having regular check-ups, individuals with atrial fibrillation can lead healthy, active lives. If you suspect you have atrial fibrillation or are at risk, consult your healthcare provider for a comprehensive evaluation and personalized management plan.