Pedal edema, the swelling of the feet and ankles, is a common symptom that can be caused by various underlying conditions. One of the primary concerns when observing pedal edema is whether it is a sign of heart failure. Heart failure is a serious condition where the heart cannot pump blood effectively, leading to a buildup of fluid in the body, including the lower extremities. Understanding the relationship between pedal edema and heart failure is crucial for early detection and management of the condition.
What Is Pedal Edema?
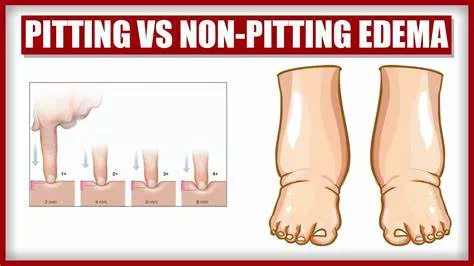
Pedal edema occurs when fluid accumulates in the tissues of the lower legs, ankles, and feet. This condition can be either pitting or non-pitting. Pitting edema is when pressing on the swollen area leaves an indentation, whereas non-pitting edema does not leave a mark. The severity of edema can vary, ranging from mild swelling to significant, noticeable changes that affect mobility and comfort.
See Also: How Long Can You Live with A Heart Stent?
Causes of Pedal Edema
Pedal edema can result from various factors, including:
Prolonged Standing or Sitting: Long periods of immobility can lead to fluid accumulation in the lower extremities due to gravity.
Injury or Surgery: Trauma or surgical procedures on the lower body can cause localized swelling.
Chronic Venous Insufficiency: This condition occurs when the veins in the legs cannot effectively return blood to the heart, leading to fluid buildup.
Kidney Disease: Impaired kidney function can result in fluid retention throughout the body, including the lower extremities.
Liver Disease: Liver disorders, such as cirrhosis, can cause fluid to accumulate in the abdomen and legs.
Lymphedema: Damage to the lymphatic system can lead to fluid accumulation in the tissues.
Pedal Edema And Heart Failure
Heart failure is a condition where the heart cannot pump blood efficiently, leading to insufficient circulation and fluid buildup. There are two main types of heart failure: left-sided and right-sided. Both can contribute to the development of pedal edema, but the mechanisms differ slightly.
Left-Sided Heart Failure
In left-sided heart failure, the left ventricle, responsible for pumping oxygenated blood to the rest of the body, fails to do so effectively. This can lead to a backup of fluid in the lungs, causing pulmonary edema. Over time, the increased pressure in the lungs can affect the right side of the heart, leading to right-sided heart failure and peripheral edema.
Right-Sided Heart Failure
Right-sided heart failure, also known as congestive heart failure, directly impacts the right ventricle’s ability to pump blood to the lungs.
This results in a backup of blood in the veins, causing fluid to leak into the tissues and leading to edema in the lower extremities. Right-sided heart failure is often a consequence of left-sided heart failure but can also occur independently due to conditions like chronic lung disease or pulmonary hypertension.
Symptoms of Heart Failure
Heart failure presents with various symptoms, and recognizing these early can help in timely diagnosis and treatment. Common symptoms include:
Shortness of Breath: Difficulty breathing, especially during physical activity or while lying flat, is a hallmark of heart failure.
Fatigue and Weakness: Reduced blood flow can lead to decreased energy levels and overall weakness.
Persistent Cough or Wheezing: Fluid buildup in the lungs can cause a chronic cough or wheezing.
Rapid or Irregular Heartbeat: Heart palpitations or an irregular heartbeat can occur as the heart tries to compensate for its reduced efficiency.
Reduced Exercise Tolerance: Individuals with heart failure often find it challenging to perform physical activities they previously managed with ease.
Swelling in the Lower Extremities: Edema in the feet, ankles, legs, and sometimes the abdomen is a common symptom.
Sudden Weight Gain: Rapid weight gain can indicate fluid retention, a sign of worsening heart failure.
Managing Pedal Edema in Heart Failure
Effective management of pedal edema involves treating the underlying heart failure and addressing the symptoms of fluid retention.
Treatment options include:
Medications:
Diuretics: These medications help the body eliminate excess fluid through urine, reducing edema.
ACE Inhibitors and ARBs: These drugs help relax blood vessels, lower blood pressure, and reduce the workload on the heart.
Beta-Blockers: These medications slow the heart rate and improve heart function.
Aldosterone Antagonists: These drugs help prevent fluid retention by blocking the effects of aldosterone, a hormone that promotes sodium and water retention.
Lifestyle Changes:
Diet: Reducing salt intake can help minimize fluid retention. A heart-healthy diet rich in fruits, vegetables, whole grains, and lean proteins is beneficial.
Exercise: Regular physical activity can improve overall cardiovascular health and help reduce edema.
Weight Management: Maintaining a healthy weight can reduce the strain on the heart.
Elevating the Legs: Elevating the legs above heart level can help reduce swelling.
Medical Devices and Surgery:
Implantable Devices: Devices such as pacemakers or defibrillators can help regulate heart rhythm and improve heart function.
Surgery: In severe cases, surgical interventions such as coronary artery bypass grafting (CABG) or heart valve repair/replacement may be necessary.
When to Seek Medical Attention
While pedal edema can have various causes, it is crucial to seek medical attention if it is accompanied by other symptoms of heart failure or if the swelling is severe and persistent. Prompt diagnosis and treatment can improve outcomes and quality of life for individuals with heart failure.
Conclusion
Pedal edema can indeed be a sign of heart failure, particularly when accompanied by other symptoms such as shortness of breath, fatigue, and rapid weight gain. Understanding the relationship between pedal edema and heart failure is essential for early detection and management of the condition. If you experience persistent swelling in your lower extremities, it is important to consult a healthcare provider for a thorough evaluation and appropriate treatment. Effective management of heart failure and its associated symptoms can significantly improve quality of life and reduce the risk of complications.