The Mechanics of Left-Sided Heart Failure
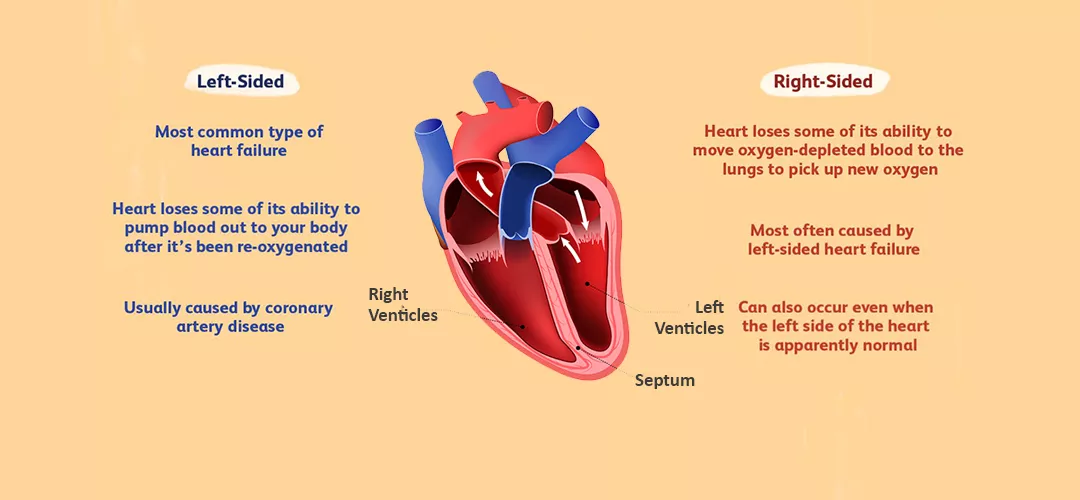
Before delving into the symptoms, it’s essential to understand the basic mechanics of left-sided heart failure. The heart comprises four chambers: two atria (upper chambers) and two ventricles (lower chambers). The left ventricle is responsible for pumping oxygenated blood from the lungs to the rest of the body. When the left ventricle fails to perform this function effectively, blood can back up into the lungs, leading to pulmonary congestion and a cascade of symptoms.
Types of Left-Sided Heart Failure
There are two main types of left-sided heart failure:
Systolic Heart Failure: This occurs when the heart muscle cannot contract forcefully enough to pump blood out effectively.
Diastolic Heart Failure: This occurs when the heart muscles become stiff and do not relax properly, leading to inadequate filling of the heart with blood between heartbeats.
See Also: Is Pedal Edema A Sign of Heart Failure
What Is The First Symptom of Left Sided Heart Failure?
Shortness of Breath: A Key Early Indicator
The first and most common symptom of left-sided heart failure is shortness of breath, medically known as dyspnea. This symptom arises due to the buildup of fluid in the lungs, a condition called pulmonary congestion or pulmonary edema.
Mechanism of Shortness of Breath
Types of Dyspnea
Other Early Symptoms of Left-Sided Heart Failure
Fatigue And Weakness
Persistent Cough or Wheezing
Fluid Retention and Swelling
Risk Factors And Causes
Hypertension (High Blood Pressure)
Coronary Artery Disease
Cardiomyopathy
Valvular Heart Disease
Diseases affecting the heart valves, such as aortic stenosis or mitral regurgitation, can cause the heart to work harder and eventually lead to left-sided heart failure.
Diabetes
Diabetes increases the risk of developing heart disease and high blood pressure, both of which are significant risk factors for heart failure.
Diagnosis And Assessment
Early diagnosis of left-sided heart failure is crucial for effective treatment and management. Several diagnostic tools and assessments can help identify the condition.
Medical History And Physical Examination
A thorough medical history and physical examination are the first steps in diagnosing heart failure. Physicians will ask about symptoms, risk factors, and family history of heart disease. During the physical exam, they will look for signs such as lung crackles (indicating fluid in the lungs), an enlarged heart, and swelling in the legs and ankles.
Imaging Tests
Echocardiogram: This ultrasound test provides detailed images of the heart’s structure and function, helping to assess the severity of heart failure and identify underlying causes.
Chest X-ray: A chest X-ray can reveal fluid in the lungs and an enlarged heart.
Magnetic Resonance Imaging (MRI): MRI can provide detailed images of the heart’s structure and function.
Blood Tests
Blood tests can help identify underlying conditions and assess the severity of heart failure. Key tests include:
B-type Natriuretic Peptide (BNP) or N-terminal pro-BNP (NT-proBNP): Elevated levels of these markers indicate heart failure.
Complete Blood Count (CBC): This test can help identify anemia, which can exacerbate heart failure symptoms.
Kidney and Liver Function Tests: These tests can assess the impact of heart failure on other organs.
Electrocardiogram (ECG)
An ECG records the electrical activity of the heart and can detect abnormalities in heart rhythm and structure that may indicate heart failure.
Treatment And Management
Early intervention and appropriate management of left-sided heart failure can improve symptoms, enhance quality of life, and prevent complications.
Medications
Several medications are used to treat heart failure, including:
Angiotensin-Converting Enzyme (ACE) Inhibitors: These drugs relax blood vessels, reduce blood pressure, and decrease the workload on the heart.
Beta-Blockers: These medications slow the heart rate and reduce blood pressure, improving heart function.
Diuretics: Diuretics help remove excess fluid from the body, reducing swelling and congestion in the lungs.
Aldosterone Antagonists: These drugs block the effects of aldosterone, a hormone that causes fluid retention.
Lifestyle Modifications
Lifestyle changes are essential for managing heart failure and improving overall health:
Diet: A heart-healthy diet low in sodium and saturated fats can help manage symptoms and improve heart function.
Exercise: Regular physical activity, as recommended by a healthcare provider, can strengthen the heart and improve circulation.
Smoking Cessation: Quitting smoking can significantly reduce the risk of heart disease and improve heart failure symptoms.
Weight Management: Maintaining a healthy weight can reduce the strain on the heart.
Monitoring And Follow-Up
Regular follow-up appointments with a healthcare provider are crucial for monitoring the condition and adjusting treatment as needed. Patients may also need to monitor their weight, blood pressure, and symptoms at home.
Conclusion
Recognizing the first symptom of left-sided heart failure, particularly shortness of breath, is vital for early diagnosis and effective management of the condition. Understanding the underlying mechanisms, risk factors, and treatment options can empower individuals and healthcare providers to take proactive steps in managing heart failure and improving patient outcomes. Early intervention, coupled with appropriate medical care and lifestyle modifications, can significantly enhance the quality of life for those living with left-sided heart failure.