Primary pulmonary hypertension (PPH), also known as idiopathic pulmonary arterial hypertension (IPAH), is a rare and progressive disorder characterized by high blood pressure in the arteries of the lungs. This increased pressure can lead to heart failure and other severe complications. Understanding the causes of primary pulmonary hypertension is essential for developing effective treatments and improving patient outcomes. In this article, we will explore the various factors and mechanisms that contribute to the development of primary pulmonary hypertension.
What Is Pulmonary Hypertension?
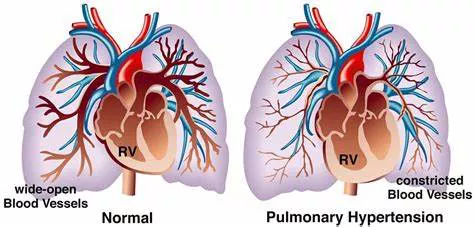
Pulmonary hypertension is a condition where the blood pressure within the pulmonary arteries—vessels that carry blood from the heart to the lungs—becomes abnormally high. There are several types of pulmonary hypertension, classified based on their underlying causes.
These include:
Pulmonary Arterial Hypertension (PAH): A group of conditions where the small arteries in the lungs become narrowed or blocked.
Pulmonary Hypertension due to Left Heart Disease: Caused by conditions affecting the left side of the heart, such as mitral valve disease or left ventricular failure.
Pulmonary Hypertension due to Lung Disease: Resulting from chronic lung diseases like chronic obstructive pulmonary disease (COPD) or interstitial lung disease.
Chronic Thromboembolic Pulmonary Hypertension (CTEPH): Caused by chronic blood clots in the lungs.
Pulmonary Hypertension with Unclear Multifactorial Mechanisms: Involves various conditions that do not fit into the other categories.
Primary pulmonary hypertension falls under the category of pulmonary arterial hypertension (PAH) and is classified as idiopathic because its exact cause is often unknown.
See Also: What is the cause of supine hypotension?
What Causes Primary Pulmonary Hypertension?
Genetic Factors
Hereditary Pulmonary Arterial Hypertension (HPAH)
One of the significant factors contributing to primary pulmonary hypertension is genetic predisposition. Hereditary PAH (HPAH) accounts for approximately 20% of idiopathic cases. Mutations in several genes have been identified as playing a crucial role in the development of the disease.
Bone Morphogenetic Protein Receptor Type 2 (BMPR2) Gene
The most well-known genetic mutation associated with primary pulmonary hypertension is in the BMPR2 gene. BMPR2 is a member of the transforming growth factor-beta (TGF-β) superfamily, which is involved in cell growth, differentiation, and apoptosis. Mutations in the BMPR2 gene disrupt normal cellular signaling and contribute to the abnormal growth of cells in the pulmonary arteries, leading to their narrowing and increased blood pressure.
Other Genetic Mutations
In addition to BMPR2, other genetic mutations have been implicated in primary pulmonary hypertension, including mutations in the ALK-1, ENG, SMAD9, and CAV1 genes. These mutations also affect pathways involved in cellular growth and vascular remodeling, contributing to the development of the disease.
Environmental and Lifestyle Factors
Exposure to Toxins and Drugs
Certain environmental and lifestyle factors can increase the risk of developing primary pulmonary hypertension. Exposure to toxins and drugs has been identified as a significant risk factor. For example, the use of appetite suppressants such as fenfluramine and dexfenfluramine has been linked to the development of primary pulmonary hypertension. Similarly, exposure to certain chemicals, such as vinyl chloride and methamphetamine, can increase the risk.
Infections
Infections, particularly those caused by the human immunodeficiency virus (HIV), have also been associated with an increased risk of primary pulmonary hypertension. HIV can lead to vascular abnormalities and increase the susceptibility to pulmonary hypertension. Other infections, such as schistosomiasis, can cause similar effects and contribute to the development of the disease.
Vascular Abnormalities
Endothelial Dysfunction
Endothelial dysfunction is a critical factor in the development of primary pulmonary hypertension. The endothelium is the inner lining of blood vessels, and its dysfunction leads to an imbalance in the production of vasoconstrictors and vasodilators. In primary pulmonary hypertension, there is an overproduction of vasoconstrictors such as endothelin-1 and a decreased production of vasodilators such as nitric oxide and prostacyclin. This imbalance results in the narrowing of pulmonary arteries and increased blood pressure.
Smooth Muscle Cell Proliferation
In addition to endothelial dysfunction, abnormal proliferation of smooth muscle cells in the pulmonary arteries plays a significant role in primary pulmonary hypertension. The abnormal growth of these cells leads to the thickening of the arterial walls, further narrowing the blood vessels and increasing blood pressure. This process is influenced by various signaling pathways and genetic mutations, including those in the BMPR2 gene.
Inflammatory and Immune Responses
Role of Inflammation
Inflammation is increasingly recognized as a contributing factor to primary pulmonary hypertension. Inflammatory cells and mediators, such as cytokines and chemokines, are often found in the lungs of patients with primary pulmonary hypertension. These inflammatory responses can lead to vascular remodeling, endothelial dysfunction, and smooth muscle cell proliferation, all of which contribute to increased pulmonary arterial pressure.
see also:What Is Congestive Gastropathy
Autoimmune Disorders
Autoimmune disorders, where the immune system attacks the body’s own tissues, have also been linked to primary pulmonary hypertension.
Conditions such as systemic sclerosis, lupus, and rheumatoid arthritis can cause vascular abnormalities and increase the risk of developing the disease. The exact mechanisms by which autoimmune disorders contribute to primary pulmonary hypertension are not fully understood but are believed to involve inflammatory and immune-mediated processes.
Hormonal Factors
Gender Differences
Primary pulmonary hypertension is more common in women than in men, suggesting that hormonal factors may play a role in its development. Estrogen, a hormone predominant in females, has been shown to influence vascular function and may contribute to the increased susceptibility to primary pulmonary hypertension in women. Research is ongoing to understand the specific mechanisms by which estrogen and other hormones impact the disease.
Pregnancy
Pregnancy can also exacerbate primary pulmonary hypertension. The increased blood volume and cardiac output during pregnancy place additional strain on the pulmonary arteries, potentially worsening the condition. Women with primary pulmonary hypertension are advised to avoid pregnancy due to the high risk of complications.
Metabolic Factors
Insulin Resistance and Metabolic Syndrome
Metabolic factors such as insulin resistance and metabolic syndrome have been associated with an increased risk of primary pulmonary hypertension. Insulin resistance can lead to endothelial dysfunction and vascular abnormalities, contributing to the development of the disease. Metabolic syndrome, characterized by a cluster of conditions including obesity, hypertension, and dyslipidemia, is also linked to an increased risk of primary pulmonary hypertension.
Obesity
Obesity is a significant risk factor for primary pulmonary hypertension.
The excess adipose tissue can lead to systemic inflammation, endothelial dysfunction, and increased pulmonary arterial pressure. Weight management and lifestyle modifications are essential in managing primary pulmonary hypertension, particularly in obese patients.
Genetic Predisposition and Family History
Familial Cases of Primary Pulmonary Hypertension
While most cases of primary pulmonary hypertension are sporadic, familial cases have been reported, suggesting a genetic predisposition.
Family history of the disease increases the risk, and genetic testing can help identify mutations associated with primary pulmonary hypertension. Understanding the genetic basis of the disease is crucial for early diagnosis and intervention.
Genetic Counseling and Testing
Genetic counseling and testing are recommended for individuals with a family history of primary pulmonary hypertension. Identifying genetic mutations can help assess the risk and guide management strategies.
Genetic counseling also provides valuable information to patients and their families regarding the inheritance patterns and implications of the disease.
Conclusion
Primary pulmonary hypertension is a complex and multifactorial disease with various contributing factors, including genetic predisposition, environmental and lifestyle factors, vascular abnormalities, inflammatory and immune responses, hormonal influences, and metabolic factors. Understanding these factors is essential for developing effective treatments and improving patient outcomes. While significant progress has been made in identifying the causes of primary pulmonary hypertension, ongoing research is needed to further elucidate the underlying mechanisms and develop targeted therapies.
Early diagnosis and intervention are crucial in managing primary pulmonary hypertension. Patients with a family history or genetic predisposition should undergo genetic counseling and testing to assess their risk. Lifestyle modifications, including weight management and avoiding exposure to toxins and drugs, can help reduce the risk of developing the disease.
Advances in understanding the genetic and molecular basis of primary pulmonary hypertension hold promise for the development of novel therapies and improved patient care.