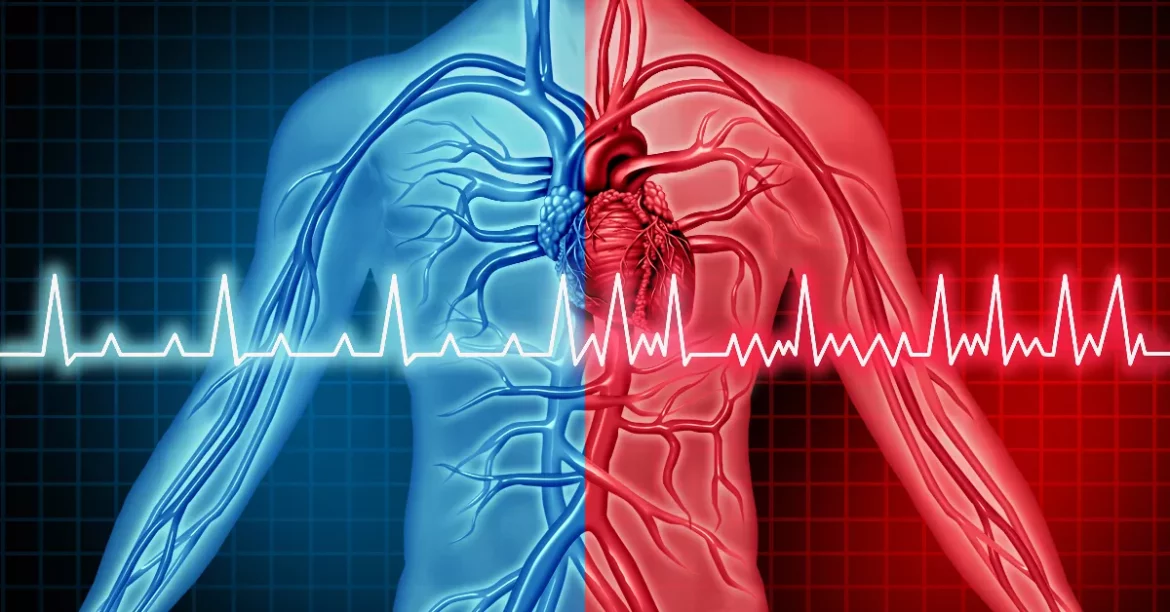
Atrial fibrillation (AFib) is a common heart condition characterized by an irregular and often rapid heartbeat. It occurs when the heart’s two upper chambers (the atria) beat out of coordination with the two lower chambers (the ventricles). This can lead to poor blood flow, causing symptoms such as palpitations, shortness of breath, and weakness. Recognizing the signs of AFib is crucial for timely intervention and management.
Common symptoms include:
- Palpitations or a racing heartbeat
- Shortness of breath
- Fatigue or weakness
- Dizziness or lightheadedness
- Chest pain or discomfort
- Anxiety
In some cases, AFib may be asymptomatic, making regular check-ups important, especially for those with risk factors like high blood pressure, heart disease, or a family history of AFib.
What to Do If Someone Has Atrial Fibrillation
When someone experiences symptoms of AFib, it’s important to act promptly. Here are the immediate steps to take:
Stay Calm: Anxiety can exacerbate the symptoms of AFib. Encourage the person to sit down and take deep, slow breaths to help calm their heart rate.
Check for Symptoms: Monitor the person’s symptoms. If they experience severe chest pain, difficulty breathing, or fainting, call emergency services immediately as these could indicate a more serious condition like a heart attack or stroke.
Monitor Heart Rate: Use a smartwatch or a heart rate monitor if available to check the heart rate. A significantly high or low heart rate can provide crucial information for healthcare professionals.
Seek Medical Attention: Even if symptoms are mild, it’s important to seek medical advice. Contact a healthcare provider to discuss the symptoms and determine if an immediate visit to the emergency room or a scheduled appointment is necessary.
see also: What to Give for Afib
Understanding Medical Evaluation And Diagnosis
Once at the healthcare facility, the medical team will perform a series of evaluations to diagnose AFib and assess its severity. The diagnostic process may include:
Electrocardiogram (ECG or EKG): This is the primary test for diagnosing AFib. It records the electrical activity of the heart and can detect irregularities in the heartbeat.
Holter Monitor: This portable device is worn for 24-48 hours to continuously monitor the heart’s activity. It’s useful for detecting intermittent AFib episodes.
Echocardiogram: This ultrasound test provides images of the heart’s structure and function, helping to identify any underlying conditions that might be causing AFib.
Blood Tests: These tests can check for conditions like thyroid disease or electrolyte imbalances that could contribute to AFib.
Stress Test: This test assesses how the heart performs under physical stress, which can help identify coronary artery disease.
Long-Term Management Strategies
Once AFib is diagnosed, the focus shifts to long-term management to control symptoms and prevent complications such as stroke and heart failure. Management strategies include:
1. Medication Management
Rate Control Medications: These medications, such as beta-blockers and calcium channel blockers, help slow down the heart rate.
Rhythm Control Medications: Antiarrhythmic drugs like flecainide or amiodarone can help restore and maintain a normal heart rhythm.
Anticoagulants: Blood thinners like warfarin, dabigatran, rivaroxaban, or apixaban reduce the risk of stroke by preventing blood clots.
2. Lifestyle Modifications
Diet: A heart-healthy diet rich in fruits, vegetables, whole grains, and lean proteins can improve overall cardiovascular health. Reducing salt, sugar, and saturated fats is crucial.
Exercise: Regular, moderate exercise helps maintain a healthy weight and improves heart function. Consult a doctor before starting any new exercise regimen.
Stress Management: Techniques such as yoga, meditation, and deep-breathing exercises can help manage stress, which may trigger AFib episodes.
Avoiding Triggers: Identifying and avoiding triggers such as excessive caffeine, alcohol, and smoking can help reduce the frequency of AFib episodes.
3. Medical Procedures
In some cases, medications and lifestyle changes may not be sufficient to control AFib. Several medical procedures can be considered:
Cardioversion: This procedure uses electrical shocks to restore a normal heart rhythm. It can be done as an emergency procedure or scheduled ahead of time.
Catheter Ablation: A minimally invasive procedure where a catheter is used to destroy the heart tissue causing the irregular rhythm. It is often considered when medication is ineffective.
Pacemaker: A device implanted under the skin to help regulate the heart’s rhythm. It is particularly useful for patients with slow heart rates.
Surgical Ablation (Maze Procedure): In severe cases, surgery might be necessary to create scar tissue that blocks the erratic electrical signals.
see also: What Can You Do for Heart Arrhythmia
Preventing Complications
Preventing complications is a critical aspect of managing AFib. Here are key measures to take:
1. Stroke Prevention
Medication Adherence: Strictly following the prescribed anticoagulant regimen is essential to prevent blood clots and reduce the risk of stroke.
Regular Monitoring: Regular blood tests to monitor clotting levels (INR for those on warfarin) ensure that the medication is working effectively.
2. Heart Failure Prevention
Weight Management: Maintaining a healthy weight reduces the strain on the heart.
Blood Pressure Control: Keeping blood pressure within a normal range is crucial to prevent further damage to the heart.
Regular Check-Ups: Routine visits to the cardiologist help monitor heart function and adjust treatment as needed.
3. Lifestyle Adjustments
Healthy Diet: Adopting a diet that supports heart health, including reducing sodium intake to prevent fluid retention and hypertension.
Alcohol Moderation: Limiting alcohol consumption can help prevent AFib episodes. If alcohol is a trigger, abstinence may be necessary.
Stress Reduction: Implementing stress management techniques can reduce the frequency and severity of AFib episodes.
Living with Atrial Fibrillation
Living with AFib requires ongoing management and adaptation. Here are some tips for day-to-day life with AFib:
1. Educate Yourself
Understanding AFib and its triggers can empower patients to manage their condition more effectively. Resources such as patient education materials from reputable organizations like the American Heart Association can be valuable.
2. Support System
Building a support network of family, friends, and healthcare providers can provide emotional support and practical assistance. Joining a support group for individuals with AFib can also offer a sense of community and shared experiences.
3. Medication Management
Keeping a medication schedule and using tools like pill organizers or reminders can help ensure adherence to treatment plans. Discuss any side effects with a healthcare provider to adjust medications if necessary.
4. Regular Monitoring
Regularly monitoring heart rate and blood pressure at home can help detect any changes that need medical attention.
Keeping a log of symptoms and triggers can provide useful information for healthcare providers.
Conclusion
Atrial fibrillation is a manageable condition with the right approach and resources. Prompt recognition of symptoms, immediate medical evaluation, and a comprehensive management plan involving medication, lifestyle changes, and possibly medical procedures can significantly improve outcomes. By understanding the condition and working closely with healthcare providers, individuals with AFib can lead active, fulfilling lives while minimizing the risk of complications.