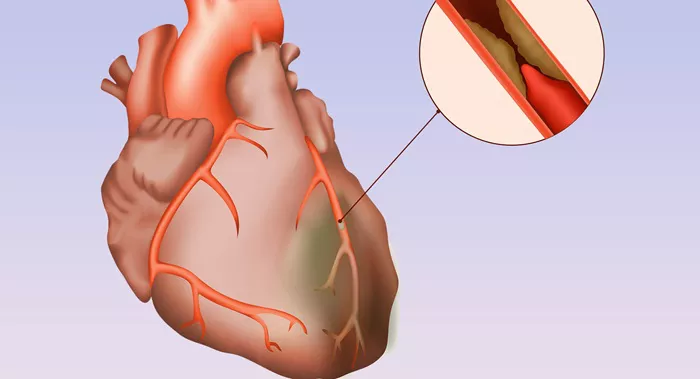
Ischemic heart disease (IHD), also known as coronary artery disease (CAD), is a condition characterized by reduced blood flow to the heart muscle due to the narrowing or blockage of the coronary arteries. This can lead to chest pain (angina), heart attacks, and other serious cardiovascular complications. Treating ischemic heart disease involves a combination of lifestyle changes, medications, and sometimes medical procedures or surgery. This article explores seven effective ways to manage and treat ICD ischemic heart disease.
7 Ways to Treat ICD Ischemic Heart Disease
1. Lifestyle Modifications
One of the most effective ways to manage ischemic heart disease is through lifestyle changes. These modifications can significantly reduce the risk factors associated with the disease and improve overall heart health.
Dietary Changes
Adopting a heart-healthy diet is crucial. This includes consuming a variety of fruits, vegetables, whole grains, lean proteins, and healthy fats such as those found in fish, nuts, and olive oil. Reducing the intake of saturated fats, trans fats, cholesterol, sodium, and added sugars is also essential.
SEE ALSO: ischemic heart disease dietary management
Exercise
Regular physical activity helps improve cardiovascular fitness, reduce blood pressure, and manage weight. The American
Heart Association recommends at least 150 minutes of moderate-intensity aerobic exercise per week, along with muscle-strengthening activities on two or more days per week.
Smoking Cessation
Smoking is a major risk factor for ischemic heart disease. Quitting smoking can significantly reduce the risk of heart attacks and other cardiovascular events. There are various smoking cessation programs and aids available, such as nicotine replacement therapy and prescription medications, to help individuals quit.
2. Medications
Medications play a critical role in managing ischemic heart disease. They help control symptoms, reduce the risk of heart attacks, and improve overall heart function. Here are some commonly prescribed medications for ICD ischemic heart disease:
Antiplatelet Agents
Aspirin and other antiplatelet medications help prevent blood clots from forming in the arteries, reducing the risk of heart attacks and strokes.
Statins
Statins are cholesterol-lowering drugs that help reduce the levels of low-density lipoprotein (LDL) cholesterol, often referred to as “bad” cholesterol. Lowering LDL cholesterol can help prevent the progression of artery blockages.
Beta-Blockers
Beta-blockers reduce the heart’s workload by slowing the heart rate and lowering blood pressure. They are commonly prescribed to manage angina and reduce the risk of future heart attacks.
ACE Inhibitors and ARBs
Angiotensin-converting enzyme (ACE) inhibitors and angiotensin II receptor blockers (ARBs) help relax blood vessels, lower blood pressure, and reduce the strain on the heart. They are often prescribed for patients with heart failure or those who have had a heart attack.
Nitroglycerin
Nitroglycerin is a medication that helps relieve angina by relaxing and widening blood vessels, improving blood flow to the heart muscle.
3. Percutaneous Coronary Intervention (PCI)
Percutaneous coronary intervention, also known as angioplasty, is a minimally invasive procedure used to open blocked or narrowed coronary arteries. This procedure involves the insertion of a catheter with a balloon at its tip into the affected artery. Once in place, the balloon is inflated to widen the artery, and a stent (a small wire mesh tube) is often inserted to keep the artery open.
Stenting
Stenting is commonly performed during PCI. The stent helps prevent the artery from narrowing again, reducing the risk of future blockages. Drug-eluting stents, which are coated with medication to prevent scar tissue from forming, are often used to improve long-term outcomes.
4. Coronary Artery Bypass Grafting (CABG)
Coronary artery bypass grafting is a surgical procedure used to treat severe blockages in the coronary arteries. During CABG, a surgeon takes a healthy blood vessel from another part of the body, such as the leg or chest, and uses it to create a new pathway for blood to flow around the blocked artery.
Benefits of CABG
CABG can significantly improve blood flow to the heart, reduce angina, and increase the patient’s ability to engage in physical activities. It is often recommended for patients with multiple blockages or those who do not respond well to other treatments.
5. Enhanced External Counterpulsation (EECP)
Enhanced external counterpulsation is a non-invasive treatment that can help improve blood flow to the heart. EECP involves the use of inflatable cuffs placed around the legs. These cuffs inflate and deflate in sync with the patient’s heartbeat, helping to increase blood flow to the coronary arteries.
EECP Benefits
EECP has been shown to reduce angina symptoms, improve exercise tolerance, and enhance the overall quality of life in patients with ischemic heart disease. It is often used for patients who are not candidates for invasive procedures or who continue to experience symptoms despite other treatments.
6. Cardiac Rehabilitation
Cardiac rehabilitation is a comprehensive program designed to help patients recover from heart-related events and improve their overall heart health. The program typically includes supervised exercise, education on heart-healthy living, and counseling to help manage stress and other risk factors.
Components of Cardiac Rehabilitation
Exercise Training: Tailored exercise programs help patients regain strength, improve cardiovascular fitness, and reduce the risk of future heart events.
Education: Patients learn about heart-healthy lifestyle changes, including dietary modifications, weight management, and smoking cessation.
Counseling: Psychological support and stress management techniques help patients cope with the emotional impact of heart disease and promote overall well-being.
7. Management of Comorbid Conditions
Many patients with ischemic heart disease also have other medical conditions that can impact their heart health. Managing these comorbid conditions is crucial for reducing the risk of complications and improving overall outcomes.
Diabetes Management
Diabetes is a major risk factor for ischemic heart disease. Effective management of blood sugar levels through medication, diet, and exercise can help reduce the risk of heart-related complications.
Hypertension Control
High blood pressure is another significant risk factor. Medications, lifestyle changes, and regular monitoring can help keep blood pressure within a healthy range, reducing the strain on the heart.
Cholesterol Management
In addition to statins, other cholesterol-lowering medications such as ezetimibe or PCSK9 inhibitors may be prescribed to help manage cholesterol levels and reduce the risk of artery blockages.
Conclusion
Managing ischemic heart disease requires a multifaceted approach that includes lifestyle modifications, medications, medical procedures, and ongoing care. By adopting heart-healthy habits, adhering to prescribed treatments, and working closely with healthcare providers, patients can effectively manage their condition and reduce the risk of serious cardiovascular events. Each patient’s treatment plan should be tailored to their specific needs and risk factors to ensure the best possible outcomes.