Cirrhosis is a severe liver disease characterized by irreversible scarring of the liver tissue, leading to compromised liver function. One of the less commonly discussed but significant complications of cirrhosis is hypotension, or low blood pressure. Understanding why cirrhosis leads to hypotension requires a comprehensive look at the complex physiological changes that occur as the disease progresses. This article delves into the mechanisms behind cirrhosis-induced hypotension, highlighting the interplay between liver dysfunction, vascular changes, and systemic effects on blood pressure regulation.
The Liver’s Role in Circulation
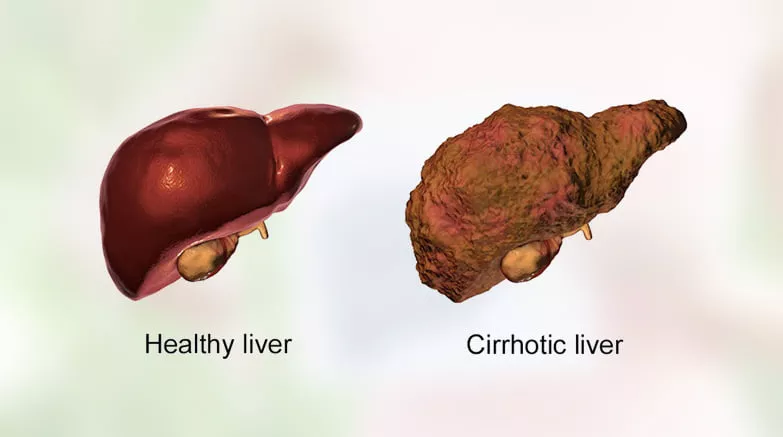
The liver is a vital organ with multifaceted functions, including metabolism, detoxification, protein synthesis, and regulation of blood volume and pressure. It produces key proteins such as albumin and clotting factors and plays a crucial role in maintaining oncotic pressure and vascular resistance. In cirrhosis, the liver’s ability to perform these functions deteriorates, leading to widespread systemic effects.
Why Does Cirrhosis Cause Hypotension?
1. Portal Hypertension and Splanchnic Vasodilation
One of the hallmark features of cirrhosis is portal hypertension, a condition where there is increased blood pressure within the portal venous system. This results from the obstruction of blood flow through the scarred liver. To compensate, the body develops collateral circulation to bypass the liver, leading to the dilation of blood vessels in the splanchnic (abdominal) circulation.
Portal hypertension triggers the release of vasodilatory substances, particularly nitric oxide, which causes the blood vessels in the splanchnic region to dilate excessively. This significant vasodilation reduces the effective blood volume returning to the heart, leading to a drop in systemic vascular resistance and consequently, hypotension.
see also: why is blood pressure low after exercise
2. Systemic Vasodilation and Hypotension
Beyond the splanchnic circulation, the vasodilatory effect of nitric oxide and other mediators can extend to the systemic circulation. Systemic vasodilation lowers peripheral vascular resistance, a major determinant of blood pressure. When peripheral resistance decreases, the blood pressure drops, leading to hypotension. This widespread vasodilation is a critical factor in the development of hypotension in patients with cirrhosis.
3. Renal Dysfunction and Hypovolemia
Cirrhosis often leads to renal dysfunction, a condition known as hepatorenal syndrome (HRS). The kidneys respond to reduced blood flow and pressure by activating the renin-angiotensin-aldosterone system (RAAS), which aims to conserve sodium and water to increase blood volume. However, in cirrhosis, this compensatory mechanism can exacerbate the problem.
Renal vasoconstriction and sodium retention result in reduced urine output and fluid overload in the body. However, this retained fluid tends to accumulate in the abdominal cavity (ascites) rather than in the vascular compartment, leading to effective hypovolemia (a decrease in the volume of circulating blood). The reduced effective arterial blood volume further lowers blood pressure, contributing to hypotension.
4. Impaired Cardiac Function
Patients with cirrhosis often exhibit cirrhotic cardiomyopathy, a condition characterized by impaired cardiac function. This condition includes features such as reduced responsiveness to stress, decreased contractility, and diastolic dysfunction. The heart’s inability to pump effectively reduces cardiac output, contributing to lower blood pressure. Additionally, the heart may struggle to compensate for the increased demand placed on it by the body’s attempts to counteract hypotension.
5. Autonomic Dysfunction
Cirrhosis is also associated with autonomic dysfunction, which affects the body’s ability to regulate blood pressure. The autonomic nervous system controls involuntary bodily functions, including blood vessel constriction and heart rate. In cirrhosis, there is often a blunted response to sympathetic nervous system activation, which normally helps to increase blood pressure in response to stress or low blood volume.
Autonomic dysfunction can impair the baroreceptor reflex, a critical mechanism for maintaining stable blood pressure.
Baroreceptors are sensors located in the blood vessels that detect changes in blood pressure and trigger compensatory mechanisms to stabilize it. In cirrhosis, the impaired baroreceptor function leads to inadequate responses to low blood pressure, perpetuating hypotension.
6. Hypoalbuminemia and Oncotic Pressure
The liver is responsible for producing albumin, a protein that plays a crucial role in maintaining oncotic pressure, which helps to keep fluid within the blood vessels. In cirrhosis, the liver’s ability to produce albumin is significantly reduced, leading to hypoalbuminemia (low levels of albumin in the blood).
Low oncotic pressure causes fluid to leak out of the blood vessels into the surrounding tissues and body cavities,a condition known as edema. This fluid shift reduces the effective blood volume within the vessels, contributing to hypotension. The loss of intravascular fluid further exacerbates the drop in blood pressure seen in cirrhosis.
7. Infection and Inflammation
Patients with cirrhosis are at an increased risk of infections, such as spontaneous bacterial peritonitis (SBP), due to compromised immune function. Infections can trigger systemic inflammatory responses, releasing cytokines and other inflammatory mediators. These mediators can cause widespread vasodilation, reduce vascular resistance, and lower blood pressure.
Sepsis, a severe and widespread infection, can lead to septic shock, characterized by dangerously low blood pressure. The combination of cirrhosis-induced hypotension and infection-related vasodilation can create a severe and life-threatening drop in blood pressure, requiring urgent medical intervention.
Management of Hypotension in Cirrhosis
Managing hypotension in patients with cirrhosis is challenging and requires a multifaceted approach. Treatment strategies aim to address the underlying causes, improve circulatory volume, and support blood pressure. Key approaches include:
Volume Expansion: Administering intravenous fluids or albumin to increase the effective blood volume and improve blood pressure.
Vasopressors: Medications such as midodrine or norepinephrine may be used to constrict blood vessels and increase blood pressure.
Addressing Ascites: Therapeutic paracentesis (draining of ascitic fluid) and diuretics to manage fluid overload and improve effective blood volume.
Renal Support: Dialysis or renal replacement therapy in severe cases of hepatorenal syndrome.
Infection Control: Prompt diagnosis and treatment of infections to prevent septic shock and further hypotension.
Monitoring and Support: Close monitoring of hemodynamic status, electrolytes, and renal function, along with supportive care in an intensive care setting if needed.
Conclusion
Hypotension in cirrhosis is a multifactorial condition arising from a complex interplay of portal hypertension, systemic vasodilation, renal dysfunction, cardiac impairment, autonomic dysfunction, hypoalbuminemia, and infection.
Understanding these mechanisms is crucial for the effective management and treatment of hypotension in cirrhotic patients. As research continues, advances in the understanding and treatment of cirrhosis and its complications may lead to improved outcomes and quality of life for affected individuals.