Aortic valve disease is a condition that can significantly impact a person’s health and quality of life. Understanding its symptoms is crucial for early detection and treatment. In this article, we will explore the various symptoms associated with aortic valve disease, providing a comprehensive overview of what to watch for.
What Is Aortic Valve Disease?
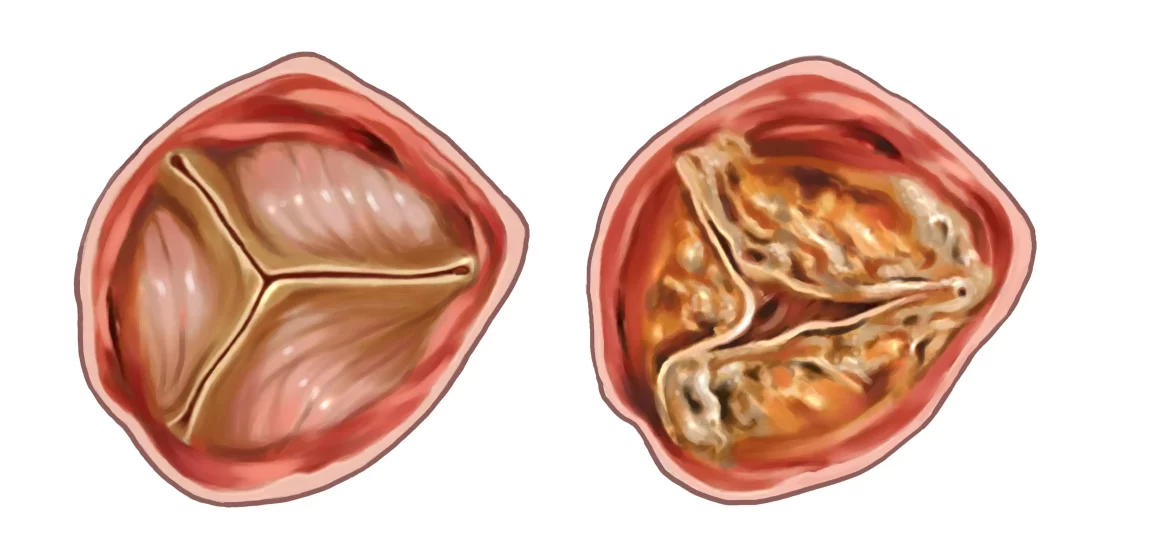
The aortic valve is a critical component of the heart, controlling blood flow from the left ventricle to the aorta and subsequently to the rest of the body. Aortic valve disease occurs when this valve malfunctions, either by not opening fully (aortic stenosis) or not closing properly (aortic regurgitation). Both conditions can lead to severe complications if left untreated.
Common Symptoms of Aortic Valve Disease
1. Chest Pain (Angina)
One of the most common symptoms of aortic valve disease is chest pain or angina. This pain typically occurs due to reduced blood flow to the heart muscles, resulting from the narrowed or malfunctioning valve. The pain can be described as a pressure, tightness, or squeezing sensation in the chest. It may also radiate to the arms, neck, jaw, or back.
SEE ALSO: How Long Can You Live with Left Heart Failure
2. Shortness of Breath
Shortness of breath, especially during physical activity, is another hallmark symptom of aortic valve disease. As the valve’s function deteriorates, the heart struggles to pump enough blood to meet the body’s demands, leading to breathlessness. In severe cases, shortness of breath may also occur at rest or when lying down.
3. Fatigue
Fatigue is a common symptom of many heart conditions, including aortic valve disease. Patients often feel unusually tired or weak, even after minimal exertion. This fatigue results from the heart’s inability to efficiently circulate blood, causing the muscles and organs to receive less oxygen and nutrients.
4. Heart Murmurs
A heart murmur is an abnormal sound heard during a heartbeat, often detected by a physician using a stethoscope. In aortic valve disease, heart murmurs occur due to turbulent blood flow through the narrowed or leaking valve. The nature and intensity of the murmur can provide clues about the severity and type of valve disease.
5. Palpitations
Palpitations, or irregular heartbeats, are another symptom that patients with aortic valve disease may experience. These can manifest as a fluttering, pounding, or racing sensation in the chest. Palpitations are often caused by the heart working harder to compensate for the valve dysfunction.
6. Dizziness and Fainting (Syncope)
Dizziness and fainting, also known as syncope, are serious symptoms that can occur in advanced cases of aortic valve disease. These episodes are typically caused by a sudden drop in blood pressure, which can result from the heart’s inability to maintain adequate circulation. Syncope is a critical warning sign that requires immediate medical attention.
7. Swelling (Edema)
Swelling, or edema, in the ankles, feet, and legs can occur in aortic valve disease due to fluid retention. As the heart’s function declines, blood flow slows, and fluid can accumulate in the tissues. This symptom is often more pronounced in the evening or after prolonged periods of standing or sitting.
Advanced Symptoms And Complications
As aortic valve disease progresses, symptoms can become more severe and lead to additional complications. It’s crucial to recognize these advanced symptoms and seek medical intervention promptly.
1. Severe Heart Failure
In advanced stages, aortic valve disease can lead to heart failure, a condition where the heart cannot pump enough blood to meet the body’s needs. Symptoms of severe heart failure include extreme fatigue, persistent coughing or wheezing, rapid weight gain due to fluid retention, and swelling in the abdomen (ascites).
2. Arrhythmias
Aortic valve disease can increase the risk of arrhythmias, which are abnormal heart rhythms. Atrial fibrillation (AFib) is a common arrhythmia associated with valve disease, characterized by rapid and irregular heartbeats. AFib can lead to blood clots, stroke, and other serious complications.
3. Endocarditis
Patients with aortic valve disease are at an increased risk of developing endocarditis, an infection of the heart’s inner lining or valves. Symptoms of endocarditis include fever, chills, night sweats, fatigue, muscle and joint pain, and unexplained weight loss. Endocarditis is a medical emergency that requires prompt treatment.
4. Sudden Cardiac Arrest
In rare cases, severe aortic valve disease can lead to sudden cardiac arrest, where the heart abruptly stops functioning. This life-threatening event requires immediate emergency medical attention and can be fatal if not treated promptly.
Diagnosing Aortic Valve Disease
Early detection and diagnosis of aortic valve disease are crucial for effective management and treatment. Several diagnostic tools and tests are used to identify and evaluate the condition:
1. Physical Examination
A thorough physical examination, including listening to the heart with a stethoscope, is often the first step in diagnosing aortic valve disease. The presence of a heart murmur can indicate valve dysfunction and prompt further investigation.
2. Echocardiogram
An echocardiogram is a key diagnostic tool for aortic valve disease. This non-invasive test uses ultrasound waves to create detailed images of the heart and its valves, allowing physicians to assess the severity and type of valve disease.
3. Electrocardiogram (ECG or EKG)
An electrocardiogram records the electrical activity of the heart and can help identify arrhythmias, heart enlargement, and other abnormalities associated with aortic valve disease.
4. Chest X-Ray
A chest X-ray provides images of the heart and lungs, helping to detect signs of heart enlargement, fluid buildup, and other related conditions.
5. Cardiac Catheterization
Cardiac catheterization involves inserting a thin tube into a blood vessel and guiding it to the heart to measure pressure and blood flow. This invasive procedure provides detailed information about the heart’s function and the severity of valve disease.
6. MRI and CT Scans
Magnetic resonance imaging (MRI) and computed tomography (CT) scans can provide detailed images of the heart and aortic valve, helping to evaluate the extent of disease and plan appropriate treatment.
Treatment Options for Aortic Valve Disease
The treatment of aortic valve disease depends on the severity of symptoms and the specific type of valve dysfunction. Options range from lifestyle changes and medications to surgical interventions.
1. Medications
Medications can help manage symptoms and improve heart function in patients with aortic valve disease. These may include:
Diuretics: To reduce fluid retention and swelling.
Beta-blockers: To manage high blood pressure and heart rate.
ACE inhibitors: To relax blood vessels and improve blood flow.
Anticoagulants: To prevent blood clots in patients with arrhythmias.
2. Lifestyle Changes
Lifestyle modifications can play a significant role in managing aortic valve disease. These include:
Regular Exercise: Engaging in moderate physical activity to improve cardiovascular health.
Healthy Diet: Following a heart-healthy diet rich in fruits, vegetables, whole grains, and lean proteins.
Smoking Cessation: Quitting smoking to reduce the risk of complications.
Weight Management: Maintaining a healthy weight to reduce the burden on the heart.
3. Surgical Interventions
In cases of severe aortic valve disease, surgical intervention may be necessary. The most common surgical options include:
Aortic Valve Replacement: Replacing the diseased valve with a mechanical or biological valve.
Aortic Valve Repair: Repairing the existing valve to improve its function.
Transcatheter Aortic Valve Replacement (TAVR): A minimally invasive procedure to replace the valve without open-heart surgery.
4. Regular Monitoring
Patients with aortic valve disease require regular follow-up appointments with their healthcare provider to monitor the condition and adjust treatment as needed. This may include periodic echocardiograms and other diagnostic tests.
Conclusion
Aortic valve disease is a serious condition that can significantly impact a person’s health and quality of life. Recognizing the symptoms is crucial for early detection and effective treatment. Common symptoms include chest pain, shortness of breath, fatigue, heart murmurs, palpitations, dizziness, fainting, and swelling. Advanced symptoms and complications can include severe heart failure, arrhythmias, endocarditis, and sudden cardiac arrest.
Early diagnosis and appropriate treatment, including medications, lifestyle changes, and surgical interventions, can help manage the condition and improve outcomes. Regular monitoring and follow-up care are essential to ensure the best possible quality of life for patients with aortic valve disease. If you or a loved one experiences any of these symptoms, it is important to seek medical attention promptly to receive a proper diagnosis and treatment plan.