Cardiomyopathy is a complex heart condition characterized by abnormal heart muscle function. It can lead to various symptoms such as fatigue, shortness of breath, chest pain, and in severe cases, heart failure. Treating cardiomyopathy requires a comprehensive approach that often involves lifestyle changes, medications, and in some cases, medical procedures. In this article, we will delve into the most common treatment options for cardiomyopathy, exploring their effectiveness, benefits, and potential risks.
What Is Cardiomyopathy?
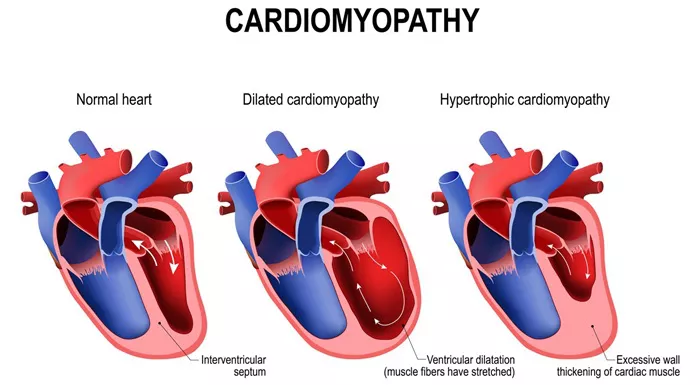
Before diving into treatment options, let’s briefly understand what cardiomyopathy entails. Cardiomyopathy is a disease that affects the heart muscle, causing it to become enlarged, thickened, or rigid. This can impair the heart’s ability to pump blood effectively, leading to symptoms like fatigue, swelling in the legs, and shortness of breath, especially during physical activity.
There are several types of cardiomyopathy, including:
Dilated Cardiomyopathy (DCM): This type is characterized by an enlarged and weakened left ventricle, which hinders the heart’s pumping ability.
Hypertrophic Cardiomyopathy (HCM): In HCM, the heart muscle becomes abnormally thick, making it harder for the heart to pump blood.
Restrictive Cardiomyopathy (RCM): RCM involves stiffening of the heart muscle, leading to reduced ventricular filling and cardiac output.
Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC): ARVC affects the right ventricle, leading to abnormal heart rhythms and potential risk of sudden cardiac arrest.
SEE ALSO: What Is The Most Common Symptom of Right Heart Failure
What Is The Most Common Treatment for Cardiomyopathy
The treatment approach for cardiomyopathy varies based on the type, severity of symptoms, and individual patient factors.
However, there are common strategies used across different types of cardiomyopathy.
Lifestyle Modifications
One of the foundational aspects of managing cardiomyopathy is making lifestyle changes that promote heart health. These include:
Dietary Modifications: Adopting a heart-healthy diet low in saturated fats, cholesterol, and sodium can help manage cardiomyopathy. Emphasizing fruits, vegetables, whole grains, lean proteins, and healthy fats like omega-3 fatty acids is beneficial.
Regular Exercise: Engaging in regular physical activity, as recommended by a healthcare provider, can improve heart function, strengthen muscles, and enhance overall well-being. However, exercise intensity and duration should be tailored to individual capabilities and limitations.
Smoking Cessation: Quitting smoking is crucial for individuals with cardiomyopathy as smoking can exacerbate heart disease and increase the risk of complications.
Alcohol Moderation: Limiting alcohol consumption or avoiding it altogether is advised, as excessive alcohol intake can contribute to heart muscle damage.
Medications
Medications play a vital role in managing cardiomyopathy by addressing symptoms, improving heart function, and preventing complications. Some common medications used in the treatment of cardiomyopathy include:
Angiotensin-Converting Enzyme (ACE) Inhibitors: These medications help dilate blood vessels, reduce blood pressure, and improve heart function by reducing the workload on the heart.
Beta-Blockers: Beta-blockers can slow the heart rate, decrease blood pressure, and improve heart function, particularly in cases of dilated cardiomyopathy.
Diuretics: Diuretics, also known as water pills, help eliminate excess fluid from the body, reducing swelling (edema) and easing the workload on the heart.
Antiarrhythmic Drugs: For individuals with cardiomyopathy associated with abnormal heart rhythms (arrhythmias), antiarrhythmic medications may be prescribed to control heart rhythm.
In addition to these medications, other drugs such as aldosterone antagonists, anticoagulants (blood thinners), and inotropes (drugs that strengthen heart contractions) may be used in specific cases based on the patient’s condition and needs.
Implantable Devices
In advanced cases of cardiomyopathy, implantable devices may be recommended to support heart function and prevent sudden cardiac events. These devices include:
Implantable Cardioverter-Defibrillator (ICD): An ICD is a device implanted under the skin that monitors heart rhythm. It can deliver electric shocks or pacing signals to restore normal heart rhythm and prevent sudden cardiac arrest.
Cardiac Resynchronization Therapy (CRT) Devices: CRT devices, also known as biventricular pacemakers, can improve heart function by coordinating the contractions of the heart’s ventricles, particularly in cases of heart failure with electrical dyssynchrony.
Left Ventricular Assist Devices (LVADs): In severe heart failure cases, an LVAD may be implanted to help the heart pump blood more effectively. LVADs are often used as a bridge to heart transplantation in eligible candidates.
Surgical Interventions
In some situations, surgical procedures may be necessary to address specific issues related to cardiomyopay. These may include:
Septal Myectomy: This surgical procedure is performed in cases of hypertrophic cardiomyopathy to remove a portion of the thickened heart muscle (septum) that obstructs blood flow.
Heart Transplantation: For individuals with end-stage heart failure due to cardiomyopathy, heart transplantation may be considered as a definitive treatment option, providing a new, healthy heart to replace the diseased one.
Alcohol Septal Ablation: Similar to septal myectomy, alcohol septal ablation involves injecting alcohol into a specific artery to reduce septal thickness in hypertrophic cardiomyopathy patients.
Lifestyle Management And Ongoing Care
Beyond initial treatment interventions, managing cardiomyopathy requires ongoing monitoring, lifestyle management, and regular medical follow-ups. Patients are encouraged to:
Monitor Symptoms: Be aware of changes in symptoms such as increased fatigue, shortness of breath, swelling, or irregular heartbeats and report them promptly to healthcare providers.
Follow Medication Regimens: Adhere to prescribed medication regimens, including dosages and timing, as directed by healthcare professionals.
Attend Follow-up Appointments: Regularly attend follow-up appointments with cardiologists or healthcare teams to assess heart function, adjust treatment plans as needed, and address any concerns.
Engage in Cardiac Rehabilitation: For eligible patients, participating in cardiac rehabilitation programs can improve cardiovascular fitness, educate on heart-healthy habits, and provide emotional support.
Conclusion
In conclusion, the most common treatment for cardiomyopathy involves a multidimensional approach that includes lifestyle modifications, medications, implantable devices, and in some cases, surgical interventions. Tailoring treatment plans to individual patient needs, type of cardiomyopathy, and disease severity is essential for optimizing outcomes and improving quality of life for individuals living with this complex heart condition. Collaboration between patients, healthcare providers, and specialists is key to effectively managing cardiomyopathy and promoting heart health.
As ongoing research and advancements in cardiac care continue, new treatment modalities and therapeutic strategies may emerge, offering hope and improved outcomes for individuals affected by cardiomyopathy.