Cardiomyopathy, a term referring to diseases of the heart muscle, encompasses a range of conditions that can affect the heart’s ability to pump blood efficiently. One of the critical factors in assessing the severity and prognosis of cardiomyopathy is its mortality rate. In this article, we delve into the various types of cardiomyopathy and explore the factors that influence mortality rates in these conditions.
What Is The Mortality Rate of Cardiomyopathy?
While specific mortality rates vary depending on the type and stage of cardiomyopathy, studies provide insights into the overall risk:
For hypertrophic cardiomyopathy, mortality rates range from 1% to 3% per year, with sudden cardiac death being a significant concern, especially in younger individuals.
Dilated cardiomyopathy has a higher mortality rate, ranging from 5% to 10% per year, particularly in advanced stages where heart failure and arrhythmias are more prevalent.
Restrictive cardiomyopathy, although less common, can have a mortality rate similar to or higher than dilated cardiomyopathy, especially in cases with significant diastolic dysfunction and heart failure.
SEE ALSO: How to Treat Cardiac Cough?
Types of Cardiomyopathy
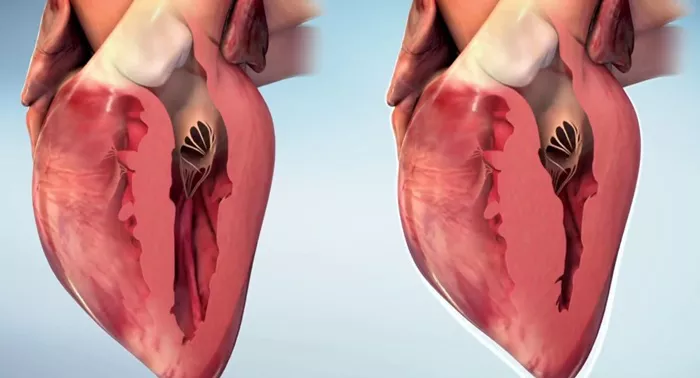
Hypertrophic Cardiomyopathy (HCM)
HCM is characterized by the thickening of the heart muscle, especially the left ventricle. This condition can obstruct blood flow and lead to symptoms like chest pain, shortness of breath, and fainting spells. The mortality rate in HCM varies depending on several factors, including the severity of the obstruction, genetic predisposition, and the presence of other cardiovascular conditions.
Dilated Cardiomyopathy (DCM)
DCM is marked by the enlargement of the heart chambers, particularly the left ventricle. This enlargement weakens the heart’s pumping ability, leading to symptoms such as fatigue, fluid retention, and arrhythmias. The mortality rate in DCM can be influenced by factors such as age, comorbidities like diabetes or hypertension, and the effectiveness of treatment interventions such as medications, lifestyle changes, and, in severe cases, heart transplantation.
Restrictive Cardiomyopathy (RCM)
RCM is characterized by stiffening of the heart muscle, which restricts its ability to fill properly with blood during the diastolic phase of the cardiac cycle. This can lead to symptoms such as exercise intolerance, fluid buildup in the legs and abdomen, and abnormal heart rhythms. The mortality rate in RCM depends on the underlying cause of the restriction, which can range from infiltrative diseases like amyloidosis to genetic factors or idiopathic origins.
Factors Influencing Mortality Rate
Disease Progression
The progression of cardiomyopathy plays a significant role in determining mortality rates. As the disease advances, the heart’s ability to function declines, increasing the risk of heart failure, arrhythmias, and other complications that can contribute to mortality.
Coexisting Conditions
Patients with cardiomyopathy often have other health conditions that can impact mortality rates. These may include diabetes, hypertension, obesity, or renal dysfunction, each adding to the complexity of managing the patient’s overall health and prognosis.
Genetic Factors
In certain types of cardiomyopathy, such as familial hypertrophic or dilated cardiomyopathy, genetic factors can influence disease progression and outcomes. Genetic testing and counseling play crucial roles in assessing risk and providing personalized treatment strategies.
Treatment Effectiveness
The effectiveness of treatment modalities, including medications, implantable devices like pacemakers or defibrillators, and surgical interventions such as heart transplantation, can significantly impact mortality rates. Timely diagnosis and appropriate management are key to improving outcomes.
Conclusion
The mortality rate of cardiomyopathy is influenced by a complex interplay of factors, including disease type, progression, comorbidities, genetic predisposition, and treatment efficacy. Timely diagnosis, comprehensive management strategies, and ongoing monitoring are essential in improving outcomes and reducing mortality rates in patients with cardiomyopathy.
Collaborative efforts between patients, healthcare providers, and researchers continue to advance our understanding and approach to managing these challenging cardiac conditions.