Diastolic dysfunction is a condition where the heart’s ability to relax and fill with blood is impaired. Unlike systolic dysfunction, which involves problems with the heart’s ability to contract and pump blood, diastolic dysfunction is concerned with the relaxation phase of the cardiac cycle. Diastolic dysfunction can lead to diastolic heart failure if it progresses, making early detection and management crucial.
Diastolic Dysfunction: Mechanisms And Causes
Diastolic dysfunction occurs when the left ventricle (LV) has difficulty relaxing and filling with blood. This can result from various mechanisms, including:
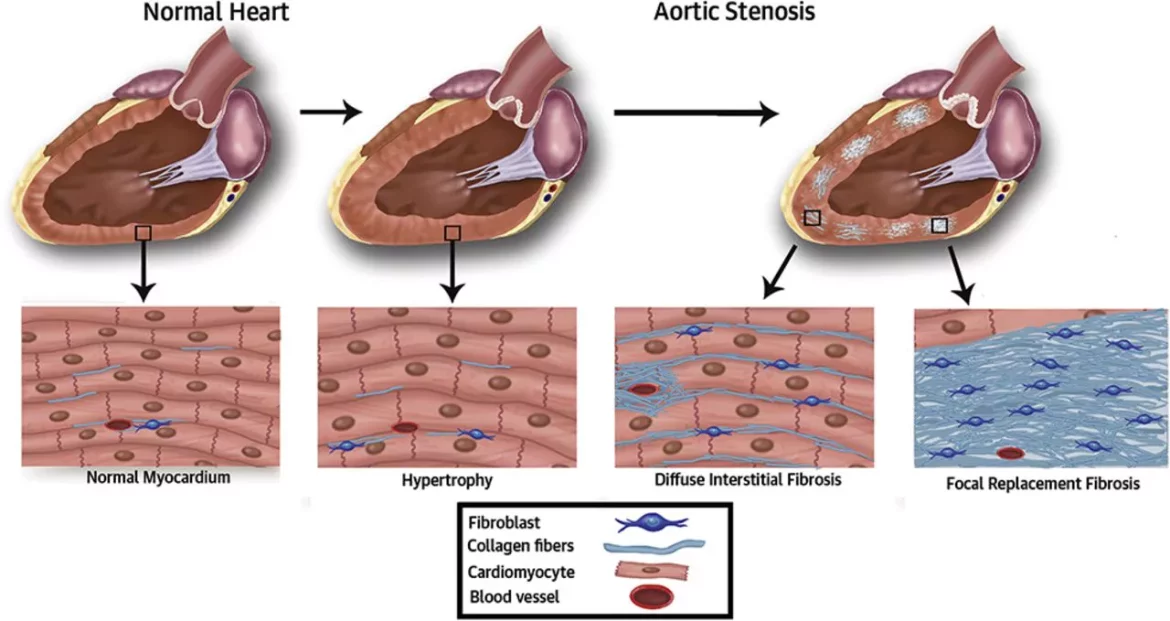
Increased Left Ventricular Stiffness: Conditions like hypertension and aortic stenosis can increase the stiffness of the left ventricle, making it harder for the heart to relax properly during diastole.
Myocardial Fibrosis:Chronic conditions such as diabetes and ischemic heart disease can lead to fibrosis (scarring) of the heart muscle, reducing its elasticity and impairing relaxation.
Altered Calcium Handling: Calcium plays a crucial role in muscle contraction and relaxation. Abnormalities in calcium handling within the heart muscle cells can disrupt normal diastolic function.
Aging: As people age, the heart’s ability to relax diminishes naturally. This age-related decline can contribute to diastolic dysfunction.
SEE ALSO: What Is Dilated Cardiomyopathy with Myocarditis?
Identifying Stage 1 Diastolic Dysfunction
Diastolic dysfunction is typically classified into stages based on the severity of impairment. Stage 1 diastolic dysfunction, also known as mild diastolic dysfunction, is the earliest and least severe form. In this stage, the heart’s ability to relax is slightly impaired, but it can still compensate by increasing the left atrial pressure to maintain adequate filling of the left ventricle.
Clinical Features of Stage 1 Diastolic Dysfunction
Stage 1 diastolic dysfunction is often asymptomatic, meaning individuals may not experience noticeable symptoms.
However, it can be detected through diagnostic tests, such as:
Echocardiography: An echocardiogram is a key diagnostic tool for identifying diastolic dysfunction. It uses ultrasound waves to create images of the heart and assess its function. Specific parameters, such as the E/A ratio (early to late ventricular filling velocities), can indicate the presence of diastolic dysfunction.
Doppler Imaging: Doppler imaging, a component of echocardiography, measures the flow of blood through the heart’s chambers and valves. It provides information about the velocity and pattern of blood flow, helping to identify diastolic dysfunction.
Left Atrial Size: Enlargement of the left atrium on echocardiography can be an indirect sign of diastolic dysfunction, as it reflects increased pressure due to impaired filling of the left ventricle.
Pathophysiology of Stage 1 Diastolic Dysfunction
In stage 1 diastolic dysfunction, the heart compensates for the impaired relaxation by increasing the left atrial pressure.
This mechanism helps maintain adequate ventricular filling and cardiac output. However, this compensatory mechanism can lead to increased left atrial size and pressure over time, potentially progressing to more severe stages of diastolic dysfunction and heart failure.
Risk Factors for Diastolic Dysfunction
Several risk factors can contribute to the development of diastolic dysfunction, including:
Hypertension: Chronic high blood pressure increases the workload on the heart, leading to left ventricular hypertrophy and stiffness.
Diabetes: Diabetes can cause myocardial fibrosis and alter calcium handling, impairing diastolic function.
Obesity: Excess body weight is associated with increased cardiac workload and changes in heart structure and function.
Coronary Artery Disease: Ischemic heart disease can damage the heart muscle and lead to fibrosis, impairing relaxation.
Aging: Age-related changes in the heart muscle and vasculature can contribute to diastolic dysfunction.
Management And Treatment of Stage 1 Diastolic Dysfunction
While stage 1 diastolic dysfunction is often asymptomatic, early detection and management are crucial to prevent progression to more severe stages and heart failure. Management strategies include:
Lifestyle Modifications: Adopting a heart-healthy lifestyle is essential for managing diastolic dysfunction. This includes:
Diet: A balanced diet rich in fruits, vegetables, whole grains, and lean proteins can help manage risk factors like hypertension, diabetes, and obesity.
Exercise: Regular physical activity can improve cardiovascular health, reduce blood pressure, and promote weight management.
Weight Management: Maintaining a healthy weight reduces the burden on the heart and improves overall cardiovascular health.
Blood Pressure Control: Managing hypertension is critical in preventing further cardiac damage. Medications such as ACE inhibitors, ARBs, and diuretics can help control blood pressure.
Blood Sugar Control: For individuals with diabetes, maintaining optimal blood sugar levels through diet, exercise, and medication can prevent myocardial fibrosis and diastolic dysfunction.
Medications: In some cases, medications may be prescribed to improve diastolic function and manage associated conditions. These may include:
Beta-Blockers: These medications can reduce heart rate and blood pressure, improving diastolic filling.
Calcium Channel Blockers: These drugs help relax the heart muscle and improve diastolic function.
Aldosterone Antagonists: These medications can reduce fibrosis and improve heart muscle relaxation.
Monitoring and Follow-Up: Regular follow-up with a healthcare provider is essential for monitoring the progression of diastolic dysfunction and adjusting treatment as needed. Echocardiography and other diagnostic tests may be used to assess heart function over time.
Conclusion
Diastolic dysfunction stage 1 is a condition characterized by impaired relaxation of the left ventricle, leading to increased left atrial pressure to maintain adequate filling. While often asymptomatic, it can be detected through diagnostic tests such as echocardiography and Doppler imaging. Managing underlying risk factors, such as hypertension and diabetes, through lifestyle modifications and medication can help prevent progression to more severe stages. Early detection and proactive management are key to improving outcomes and maintaining cardiovascular health in individuals with diastolic dysfunction stage 1.