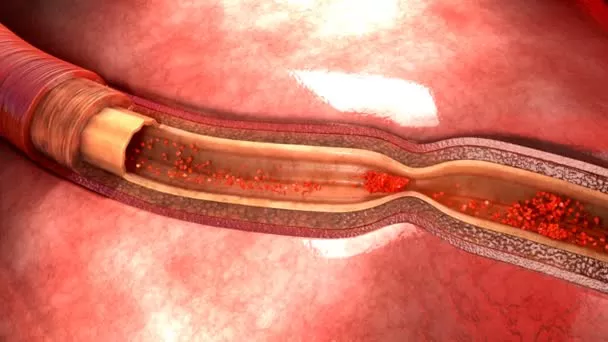
A vascular spasm, also known as vasospasm, refers to the sudden constriction of a blood vessel, reducing its diameter and restricting blood flow. This phenomenon can occur in any blood vessel, including arteries and veins, but it is most commonly associated with coronary arteries, which supply blood to the heart muscle. Vascular spasms can lead to various medical conditions, depending on their location and severity, and can be a precursor to serious cardiovascular events such as heart attacks.
Mechanism of Vascular Spasms
The exact mechanism behind vascular spasms is not fully understood, but it involves complex interactions between the endothelial cells lining the blood vessels, the smooth muscle cells in the vessel wall, and various chemical and neural signals.
Endothelial Dysfunction: The endothelium, the inner lining of blood vessels, plays a crucial role in regulating vascular tone. It produces substances like nitric oxide (NO) that help relax the smooth muscle cells. Dysfunction in the endothelium can disrupt this balance, leading to excessive constriction.
Smooth Muscle Hyperreactivity: Smooth muscle cells in the vessel walls contract in response to signals from the endothelium and nervous system. In vascular spasms, these cells may become overly reactive, contracting more than necessary.
Chemical Mediators: Various chemical mediators, such as endothelin, serotonin, and thromboxane, can induce vasoconstriction. An imbalance in these chemicals can trigger a spasm.
Nervous System Influence: The autonomic nervous system, which controls involuntary functions, can also influence vascular tone.
Overactivity of the sympathetic nervous system can contribute to spasms.
SEE ALSO: Which Fruit Is Good for Heart And Lungs?
Causes of Vascular Spasms
Vascular spasms can be triggered by a variety of factors, including:
Atherosclerosis: The buildup of plaques in the arteries can cause the endothelium to become dysfunctional, making spasms more likely.
Smoking: Nicotine and other chemicals in cigarettes can damage the endothelium and increase the risk of spasms.
Stress and Anxiety: Emotional stress can stimulate the sympathetic nervous system, leading to increased vascular tone and potential spasms.
Cold Exposure: Sudden exposure to cold temperatures can cause blood vessels to constrict.
Certain Medications: Some medications, particularly those that affect the cardiovascular system, can predispose individuals to spasms.
Cocaine Use: Cocaine is a potent vasoconstrictor and can lead to severe coronary spasms.
Symptoms of Vascular Spasms
The symptoms of vascular spasms depend on their location and the degree of blood flow restriction. In the case of coronary artery spasms, symptoms may mimic those of angina or a heart attack, including:
Chest Pain: A sudden, intense pain in the chest that may radiate to the neck, jaw, shoulders, or arms.
Shortness of Breath: Difficulty breathing or a feeling of being unable to catch one’s breath.
Palpitations: A sensation of irregular or rapid heartbeats.
Nausea and Sweating: Feeling nauseous and breaking out in a cold sweat.
Spasms in other blood vessels can cause symptoms specific to the affected area. For example, a spasm in a cerebral artery may lead to symptoms of a transient ischemic attack (TIA) or stroke, such as sudden weakness, numbness, or confusion.
Diagnosis of Vascular Spasms
Diagnosing vascular spasms involves a combination of clinical evaluation, patient history, and diagnostic tests. Key steps include:
Medical History and Physical Examination: A thorough history of symptoms, lifestyle factors (such as smoking or drug use), and family history of cardiovascular disease is essential. A physical examination can help rule out other causes of symptoms.
Electrocardiogram (ECG): An ECG can detect changes in the heart’s electrical activity that may suggest ischemia (reduced blood flow) due to spasms.
Echocardiogram: This ultrasound test provides images of the heart and can identify areas of reduced blood flow or heart muscle damage.
Coronary Angiography: This invasive test involves injecting a contrast dye into the coronary arteries and taking X-ray images to visualize blood flow and detect spasms.
Stress Tests: Exercise or pharmacological stress tests can provoke symptoms and help identify spasms.
Treatment And Management of Vascular Spasms
The treatment of vascular spasms aims to relieve symptoms, prevent recurrence, and address underlying risk factors.
Approaches include:
Medications: Several classes of drugs can help manage vascular spasms:
Calcium Channel Blockers: These drugs relax the smooth muscle in the vessel walls, reducing the likelihood of spasms.
Examples include diltiazem and amlodipine.
Nitrates: Nitroglycerin and other nitrates dilate blood vessels and can relieve chest pain associated with spasms.
Beta-Blockers: These drugs reduce the heart’s workload and decrease the risk of spasms triggered by stress.
Statins: If atherosclerosis is a contributing factor, statins can help lower cholesterol levels and improve endothelial function.
Lifestyle Changes: Modifying lifestyle factors that contribute to vascular spasms is crucial:
Quit Smoking: Smoking cessation is essential to reduce the risk of spasms and improve overall cardiovascular health.
Stress Management: Techniques such as relaxation exercises, meditation, and counseling can help manage stress and reduce the likelihood of spasms.
Healthy Diet and Exercise: A heart-healthy diet and regular physical activity can improve vascular health and reduce risk factors like hypertension and hyperlipidemia.
Avoidance of Triggers: Identifying and avoiding specific triggers, such as cold exposure or certain medications, can help prevent spasms.
Surgical Interventions: In severe cases where spasms lead to significant coronary artery disease or recurrent symptoms, surgical options like angioplasty or coronary artery bypass grafting (CABG) may be considered.
Prognosis And Complications
The prognosis for individuals with vascular spasms varies depending on the severity and frequency of the spasms, the presence of underlying cardiovascular disease, and the effectiveness of treatment. While many people can manage their condition successfully with medication and lifestyle changes, some may experience recurrent or severe spasms that increase the risk of complications.
Potential complications of untreated or severe vascular spasms include:
Myocardial Infarction (Heart Attack): Prolonged or severe spasms can lead to a heart attack by significantly restricting blood flow to the heart muscle.
Arrhythmias: Vascular spasms can disrupt the heart’s electrical activity, leading to abnormal heart rhythms.
Heart Failure: Repeated episodes of ischemia can weaken the heart muscle and lead to heart failure.
Stroke: Spasms in cerebral arteries can increase the risk of ischemic stroke.
Conclusion
Vascular spasms are a significant medical condition that can lead to serious cardiovascular events if not properly managed.
Understanding the mechanisms, causes, symptoms, and treatment options for vascular spasms is essential for both patients and healthcare providers. By addressing underlying risk factors, utilizing appropriate medications, and making lifestyle changes, individuals with vascular spasms can often lead healthy, active lives while minimizing the risk of complications.