Non-obstructive hypertrophic cardiomyopathy (HCM) is a condition characterized by the abnormal thickening of the heart muscle, specifically the ventricles, without any blockage (obstruction) of blood flow out of the heart. This can lead to various symptoms such as chest pain, shortness of breath, palpitations, and fatigue. Managing non-obstructive HCM focuses on symptom relief, improving heart function, and preventing complications.
7 Treatments for Non-Obstructive Hypertrophic Cardiomyopathy
1. Beta Blockers
Beta blockers are a class of medications commonly used to treat non-obstructive HCM. They work by slowing the heart rate and reducing the force of contraction, which can help alleviate symptoms such as chest pain and palpitations.
Mechanism of Action:
Beta blockers block the effects of adrenaline on the heart, reducing heart rate and blood pressure. This decreases the heart’s demand for oxygen and reduces the risk of arrhythmias.
Common Beta Blockers:
- Metoprolol
- Atenolol
- Propranolol
Benefits:
Beta blockers can significantly improve symptoms and enhance exercise tolerance. They are often the first-line treatment for patients with non-obstructive HCM.
see also: What to Do When Cardiac Ablation Fails?
Side Effects:
Potential side effects include fatigue, dizziness, and cold extremities.
It’s important to start with a low dose and gradually increase it to minimize these effects.
2. Calcium Channel Blockers
Calcium channel blockers are another class of medications that can be effective in treating non-obstructive HCM. They help to relax the heart muscle and improve blood flow.
Mechanism of Action:
These medications inhibit the influx of calcium ions into cardiac muscle cells, leading to a decrease in muscle contraction strength and relaxation of the blood vessels.
Common Calcium Channel Blockers:
- Verapamil
- Diltiazem
Benefits:
Calcium channel blockers can help reduce symptoms such as chest pain and improve exercise capacity. They are especially useful in patients who do not tolerate beta blockers well.
Side Effects:
Potential side effects include constipation, dizziness, and swelling in the lower extremities. Careful monitoring is required to adjust the dosage as needed.
3. Antiarrhythmic Medications
Arrhythmias are a common complication of non-obstructive HCM.
Antiarrhythmic medications can help control abnormal heart rhythms and prevent sudden cardiac death.
Mechanism of Action:
These medications work by altering the electrical signals in the heart, stabilizing the heart rhythm and preventing arrhythmias.
Common Antiarrhythmic Medications:
- Amiodarone
- Disopyramide
- Sotalol
Benefits:
Antiarrhythmic medications can significantly reduce the risk of serious arrhythmias and improve quality of life.
Side Effects:
Side effects vary depending on the medication but can include fatigue, dizziness, and gastrointestinal issues. Long-term use of some antiarrhythmics, such as amiodarone, requires regular monitoring for potential toxicities.
4. Lifestyle Modifications
Lifestyle changes are a crucial component of managing non-obstructive HCM. These modifications can help reduce symptoms and improve overall heart health.
Recommendations:
Regular Exercise: Engaging in moderate-intensity aerobic exercise can strengthen the heart and improve cardiovascular fitness. Avoiding intense competitive sports and heavy lifting is advised to prevent undue stress on the heart.
Healthy Diet: A balanced diet rich in fruits, vegetables, whole grains, and lean proteins can support heart health. Limiting salt intake can help manage blood pressure.
Weight Management: Maintaining a healthy weight reduces the burden on the heart and can alleviate symptoms.
Benefits:
Lifestyle modifications can enhance overall well-being and complement medical treatments. They also reduce the risk of other cardiovascular conditions.
5. Implantable Cardioverter-Defibrillator (ICD)
For patients at high risk of sudden cardiac death due to arrhythmias, an implantable cardioverter-defibrillator (ICD) may be recommended.
This device monitors the heart rhythm and delivers shocks if a life-threatening arrhythmia is detected.
Mechanism of Action:
An ICD continuously monitors the heart’s electrical activity and delivers an electric shock to restore normal rhythm if it detects a dangerous arrhythmia.
Benefits:
ICDs can be life-saving by preventing sudden cardiac death. They provide peace of mind for patients and their families.
Considerations:
Implantation of an ICD involves a surgical procedure and carries risks such as infection and device malfunction. Regular follow-up is necessary to ensure the device is functioning correctly.
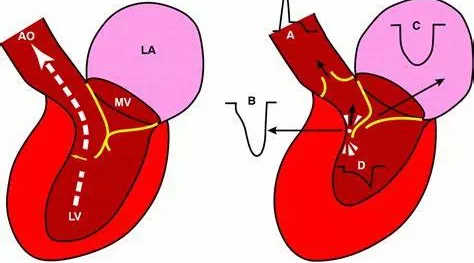
6. Septal Ablation
In some cases, septal ablation may be considered to reduce the thickness of the heart muscle. This minimally invasive procedure can help alleviate symptoms and improve heart function.
Procedure:
Septal ablation involves injecting alcohol into the arter
supplying the thickened part of the heart muscle, causing it to shrink.
Benefits:
Septal ablation can improve symptoms such as shortness of breath and chest pain. It is an alternative for patients who are not candidates for surgical myectomy.
Risks:
Potential risks include arrhythmias, heart block, and the need for a permanent pacemaker. Careful patient selection and expertise in performing the procedure are essential.
7. Surgical Myectomy
For patients with severe symptoms that do not respond to other treatments, surgical myectomy may be an option. This surgery involves removing part of the thickened heart muscle to improve blood flow and reduce symptoms.
Procedure:
During a myectomy, a surgeon removes a portion of the thickened septum, the wall between the left and right ventricles, to improve blood flow out of the heart.
Benefits:
Surgical myectomy can provide significant and long-lasting symptom relief. It can improve quality of life and exercise capacity.
Risks:
As with any surgery, there are risks involved, including infection, bleeding, and complications from anesthesia. Recovery time may vary, and patients need close postoperative monitoring.
Conclusion
Managing non-obstructive hypertrophic cardiomyopathy requires a comprehensive approach that includes medications, lifestyle modifications, and possibly interventional procedures. Beta blockers, calcium channel blockers, antiarrhythmic medications, and ICDs are essential components of the treatment plan. Additionally, lifestyle changes and interventional procedures like septal ablation and surgical myectomy can play crucial roles in alleviating symptoms and preventing complications.