Hypercapnia, the medical term for elevated levels of carbon dioxide (CO2) in the blood, is a condition that can have significant health implications. This article delves into the causes of high CO2 levels in the blood, exploring the underlying mechanisms, contributing factors, and potential health risks. Understanding these aspects is crucial for both medical professionals and patients to manage and prevent the adverse effects associated with hypercapnia.
The Role of CO2 in the Body
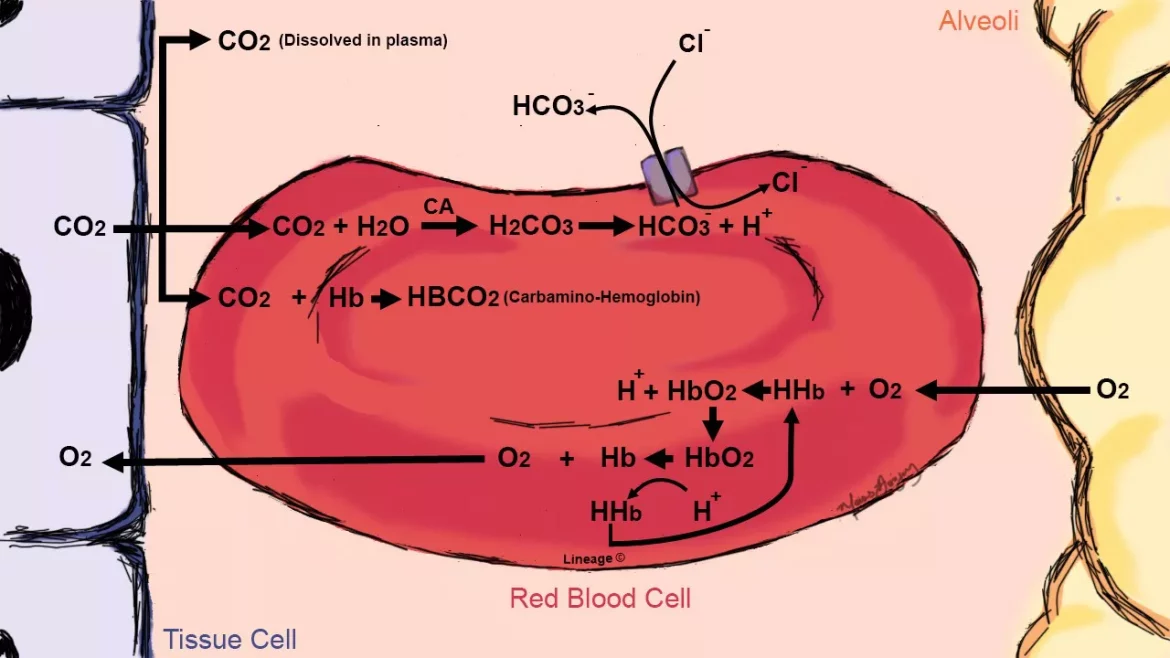
Carbon dioxide is a natural byproduct of the body’s metabolic processes. It is produced in the cells as they generate energy from nutrients through a process known as cellular respiration. The blood transports CO2 from the tissues to the lungs, where it is exhaled. This gas exchange process is vital for maintaining the body’s acid-base balance and overall homeostasis.
Mechanisms of CO2 Regulation
The body tightly regulates CO2 levels through the respiratory system. Chemoreceptors in the brain and blood vessels monitor CO2 concentrations and adjust the rate and depth of breathing to maintain optimal levels. When CO2 levels rise, these chemoreceptors stimulate an increase in respiratory rate to expel the excess gas. Conversely, when CO2 levels drop, the respiratory rate decreases.
What Causes High Levels of CO2 in Blood?
Several factors can disrupt the body’s ability to regulate CO2 levels, leading to hypercapnia. These causes can be broadly categorized into respiratory, metabolic, and external factors.
SEE AISO: What to Take for Blood Pressure Headache
Respiratory Causes
Chronic Obstructive Pulmonary Disease (COPD):
COPD, which includes chronic bronchitis and emphysema, is a leading cause of hypercapnia. In COPD, the airways and air sacs in the lungs are damaged, making it difficult to expel CO2. This results in its accumulation in the blood.
Respiratory Muscle Weakness:
Conditions like muscular dystrophy, amyotrophic lateral sclerosis (ALS), and Guillain-Barré syndrome can weaken the respiratory muscles, impairing the ability to breathe effectively and eliminate CO2.
Obstructive Sleep Apnea (OSA):
OSA is characterized by repeated episodes of partial or complete obstruction of the airway during sleep. This obstruction prevents adequate ventilation and can lead to increased CO2 levels.
Severe Asthma:
During an asthma attack, the airways become constricted, limiting airflow and causing CO2 retention.
Pulmonary Edema:
This condition involves fluid accumulation in the lungs, which impairs gas exchange and can result in elevated CO2 levels.
Metabolic Causes
Metabolic Acidosis:
Conditions such as diabetic ketoacidosis and lactic acidosis increase the production of acidic compounds in the body, which can elevate CO2 levels as the body attempts to buffer the increased acidity.
Kidney Failure:
The kidneys play a crucial role in maintaining acid-base balance. In kidney failure, the kidneys’ ability to excrete acids is compromised, leading to CO2 retention.
External Factors
Exposure to High CO2 Environments:
Situations such as working in confined spaces with poor ventilation or exposure to certain industrial environments can increase inhalation of CO2.
Use of Certain Medications:
Drugs that depress the central nervous system, such as opioids and sedatives, can reduce the drive to breathe, leading to CO2 accumulation.
Mechanical Ventilation:
Improper settings on mechanical ventilators used in critical care can result in insufficient ventilation and elevated CO2 levels.
Symptoms and Health Implications
Elevated CO2 levels in the blood can manifest through various symptoms and have serious health consequences if not addressed promptly.
Symptoms of Hypercapnia
Shortness of Breath:
Difficulty breathing or feeling breathless is a common symptom as the body struggles to expel excess CO2.
Headache:
Elevated CO2 levels can cause vasodilation in the brain, leading to headaches.
Confusion and Drowsiness:
CO2 narcosis, a state of altered consciousness, can occur as CO2 levels rise, resulting in confusion, drowsiness, and even stupor.
Flushed Skin:
Hypercapnia can cause a flushed or reddened appearance of the skin due to increased blood flow.
Increased Heart Rate:
The body compensates for high CO2 levels by increasing heart rate to enhance blood flow and oxygen delivery.
Severe Health Risks
Respiratory Failure:
If the underlying cause of hypercapnia is not addressed, it can lead to respiratory failure, a life-threatening condition requiring immediate medical intervention.
Acidosis:
Elevated CO2 levels can lead to respiratory acidosis, a condition where the blood becomes too acidic. This can affect various bodily functions and cause organ dysfunction.
Cardiovascular Complications:
Hypercapnia can increase the workload on the heart, leading to hypertension and other cardiovascular issues.
Diagnosis And Monitoring
Diagnosing hypercapnia involves a combination of clinical assessment, patient history, and diagnostic tests.
Arterial Blood Gas (ABG) Analysis
ABG analysis is the gold standard for measuring CO2 levels in the blood. This test provides information on the pH, partial pressure of CO2 (PaCO2), and oxygen levels.
Pulse Oximetry
While pulse oximetry primarily measures oxygen saturation, it can provide indirect clues about CO2 levels when used in conjunction with other assessments.
Imaging Studies
Chest X-rays, CT scans, and MRI can help identify underlying respiratory conditions contributing to hypercapnia.
Pulmonary Function Tests
These tests assess lung function and can help diagnose conditions like COPD and asthma.
Treatment And Management
The management of hypercapnia involves addressing the underlying cause and improving ventilation to lower CO2 levels.
Supplemental Oxygen Therapy
Oxygen therapy can help alleviate symptoms and improve oxygen levels in patients with respiratory conditions. However, it must be used cautiously in COPD patients to avoid further CO2 retention.
Mechanical Ventilation
In severe cases, mechanical ventilation may be necessary to support breathing and reduce CO2 levels. Settings should be carefully adjusted to ensure adequate ventilation.
Bronchodilators and Steroids
These medications can help open airways and reduce inflammation in conditions like asthma and COPD, improving airflow and CO2 clearance.
Non-Invasive Ventilation (NIV)
NIV, such as continuous positive airway pressure (CPAP) or bilevel positive airway pressure (BiPAP), can support breathing in patients with conditions like sleep apnea and COPD.
Lifestyle Modifications
Quitting smoking, maintaining a healthy weight, and avoiding exposure to pollutants can help manage and prevent hypercapnia in individuals with chronic respiratory conditions.
Prevention Strategies
Preventing hypercapnia involves managing risk factors and maintaining overall respiratory health.
Regular Medical Check-Ups
Routine check-ups can help detect and manage conditions that could lead to hypercapnia early.
Adherence to Treatment Plans
Patients with chronic respiratory conditions should adhere to prescribed treatment plans, including medications and lifestyle modifications.
Healthy Lifestyle Choices
Engaging in regular physical activity, eating a balanced diet, and avoiding smoking and excessive alcohol consumption can promote respiratory health.
Environmental Considerations
Ensuring good ventilation in living and working spaces can help prevent CO2 buildup.
Conclusion
Hypercapnia, or elevated levels of CO2 in the blood, is a complex condition with various underlying causes. Respiratory disorders, metabolic imbalances, and external factors can all contribute to this potentially serious condition. Understanding the causes, symptoms, and management strategies is essential for preventing and treating hypercapnia effectively. By addressing underlying issues and adopting healthy lifestyle practices, individuals can maintain optimal respiratory health and avoid the adverse effects of elevated CO2 levels in the blood.