Paroxysmal supraventricular tachycardia (PSVT) is a common type of arrhythmia characterized by sudden episodes of rapid heart rate originating above the ventricles. Understanding the causes of PSVT is crucial for effective diagnosis and management. This article delves into the various factors that can trigger PSVT, exploring the underlying mechanisms and potential risk factors.
Introduction to Paroxysmal Supraventricular Tachycardia
PSVT is a condition where the heart suddenly begins to beat very fast due to abnormal electrical activity. These episodes can start and stop abruptly, and the heart rate during an episode can exceed 100 beats per minute, often reaching 150-250 beats per minute. Although PSVT is usually not life-threatening, it can cause significant discomfort and may lead to more serious conditions if left untreated.
see also: 7 Symptoms of Paroxysmal Atrial Fibrillation
Key Components of The Cardiac Electrical System
Sinoatrial (SA) Node: Often referred to as the heart’s natural pacemaker, the SA node initiates electrical impulses that cause the atria to contract.
Atrioventricular (AV) Node: This node receives the impulse from the SA node and slows it down before passing it to the ventricles, ensuring that the atria have time to contract fully before the ventricles contract.
Bundle of His and Purkinje Fibers: These structures distribute the electrical impulse throughout the ventricles, causing them to contract and pump blood to the body.
Mechanisms Leading to PSVT
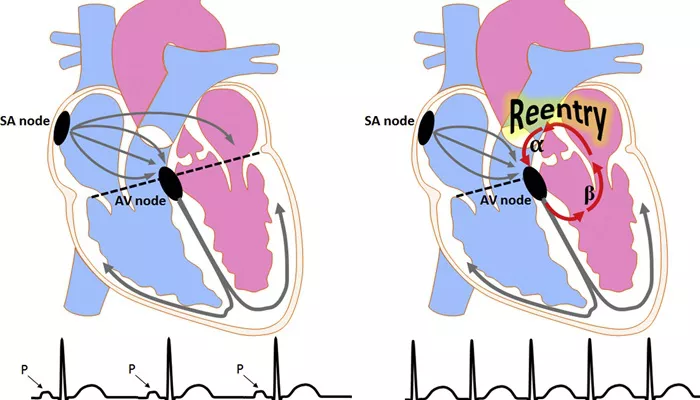
PSVT occurs when there is a disruption in the normal conduction of electrical impulses in the heart. Several mechanisms can lead to this abnormal electrical activity:
Re-entry Circuits
The most common mechanism behind PSVT is re-entry, where an electrical impulse re-enters and reactivates the heart tissue, creating a loop of continuous activity. This can occur in different parts of the heart, including:
Atrioventricular Re-entry Tachycardia (AVRT): This type involves an additional pathway connecting the atria and ventricles, known as an accessory pathway. The most well-known condition associated with AVRT is Wolff-Parkinson-White (WPW) syndrome.
Atrioventricular Nodal Re-entry Tachycardia (AVNRT): Here, the re-entry circuit is located within the AV node itself, leading to rapid and regular heartbeats.
Automaticity
Abnormal automaticity refers to the heart cells’ ability to generate electrical impulses spontaneously and at a faster rate than normal.
This can occur due to various conditions that affect the heart cells’ excitability, leading to episodes of PSVT.
Triggered Activity
Triggered activity involves afterdepolarizations, where abnormal electrical activity occurs during or after the heart’s repolarization phase. These afterdepolarizations can reach a threshold that triggers premature heartbeats, leading to PSVT.
Potential Causes And Risk Factors
Several factors can contribute to the development of PSVT. These include both intrinsic cardiac issues and external influences that affect the heart’s electrical system.
1. Cardiac Causes
Congenital Heart Defects: Structural abnormalities present at birth can disrupt the normal conduction pathways, increasing the risk of PSVT.
Previous Heart Surgery: Surgical interventions can create scar tissue in the heart, which can act as a site for re-entry circuits.
Ischemic Heart Disease: Reduced blood flow to the heart muscle can damage the conduction system, leading to arrhythmias like PSVT.
Cardiomyopathy: Diseases that affect the heart muscle can alter its electrical properties, predisposing individuals to PSVT.
2. Electrolyte Imbalances
Electrolytes such as potassium, calcium, and magnesium play crucial roles in maintaining the heart’s electrical stability.
Imbalances in these electrolytes can disrupt normal conduction and lead to PSVT.
Hypokalemia: Low potassium levels can increase the heart’s susceptibility to abnormal electrical activity.
Hyperkalemia: Excessive potassium can also disturb the heart’s rhythm, causing PSVT.
Hypocalcemia and Hypercalcemia: Abnormal calcium levels can affect the conduction system and the heart’s excitability.
Magnesium Imbalance: Both low and high levels of magnesium can influence the occurrence of arrhythmias.
3. Medications and Stimulants
Certain medications and stimulants can provoke PSVT by affecting the heart’s electrical activity or its response to stress.
Antiarrhythmic Drugs: Paradoxically, medications meant to control arrhythmias can sometimes cause or exacerbate PSVT.
Stimulants: Caffeine, nicotine, and recreational drugs like cocaine and amphetamines can increase heart rate and precipitate PSVT.
Prescription Medications: Some medications, including beta-blockers and calcium channel blockers, can lead to PSVT in certain individuals.
4. Autonomic Nervous System Imbalance
The autonomic nervous system, which controls involuntary bodily functions, plays a significant role in regulating heart rate. Imbalances between the sympathetic and parasympathetic nervous systems can trigger PSVT.
Stress and Anxiety: Emotional stress and anxiety can activate the sympathetic nervous system, leading to increased heart rate and PSVT episodes.
Vagal Tone: Excessive vagal tone, which slows the heart rate, can paradoxically lead to re-entry circuits and PSVT.
5. Hormonal Influences
Hormonal changes, particularly those involving thyroid hormones, can have a significant impact on heart rhythm.
Hyperthyroidism: Excess thyroid hormone can increase the heart rate and its susceptibility to arrhythmias, including PSVT.
Hypothyroidism: Low thyroid hormone levels can also disrupt the heart’s normal rhythm.
6. Lifestyle Factors
Certain lifestyle choices and habits can contribute to the development of PSVT.
Alcohol Consumption: Excessive alcohol intake can lead to “holiday heart syndrome,” where binge drinking triggers arrhythmias like PSVT.
Sleep Deprivation: Lack of sleep can stress the heart and increase the risk of arrhythmias.
Dehydration: Insufficient fluid intake can lead to electrolyte imbalances, increasing the likelihood of PSVT.
Diagnosis And Management
Identifying the causes of PSVT is essential for effective management.
Diagnosis typically involves a combination of patient history, physical examination, and diagnostic tests such as electrocardiograms (ECGs), Holter monitors, and electrophysiological studies.
Diagnostic Tools
Electrocardiogram (ECG): This test records the electrical activity of the heart and can identify abnormal rhythms associated with PSVT.
Holter Monitor: A portable ECG device worn for 24-48 hours to detect intermittent arrhythmias.
Event Monitor: Similar to a Holter monitor, but worn for a longer period, allowing patients to record symptoms as they occur.
Electrophysiological Study (EPS): An invasive test that maps the heart’s electrical activity to pinpoint the location of abnormal circuits.
Management Strategies
Treatment of PSVT depends on the frequency, duration, and severity of episodes, as well as the underlying cause. Options include:
Vagal Maneuvers: Simple physical actions like bearing down or applying cold water to the face can stimulate the vagus nerve and help terminate PSVT episodes.
Medications: Antiarrhythmic drugs, beta-blockers, and calcium channel blockers can help control or prevent episodes.
Catheter Ablation: A procedure that uses radiofrequency energy to destroy the abnormal tissue causing PSVT.
Lifestyle Modifications: Reducing stress, avoiding stimulants, and maintaining a healthy lifestyle can help manage PSVT.
Conclusion
Paroxysmal supraventricular tachycardia (PSVT) is a condition characterized by sudden, rapid heartbeats due to abnormal electrical activity in the heart. Understanding the causes of PSVT is crucial for accurate diagnosis and effective management. PSVT can result from various mechanisms, including re-entry circuits, abnormal automaticity, and triggered activity. Risk factors such as congenital heart defects, electrolyte imbalances, medications, autonomic nervous system imbalance, hormonal influences, and lifestyle factors can contribute to the development of PSVT.