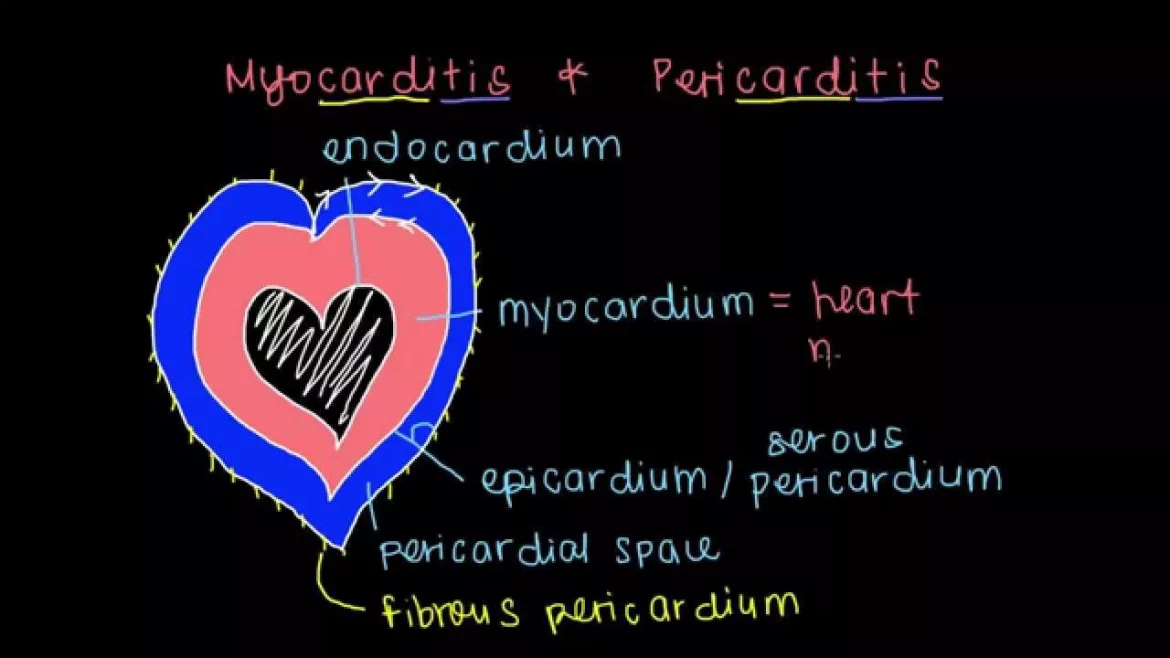
Myocarditis, an inflammation of the heart muscle, has recently garnered significant attention due to its potential association with certain vaccines, particularly those developed for COVID-19. This article delves into the relationship between vaccines and myocarditis, examining the data, understanding the risks, and dispelling myths.
The Role of Vaccines in Preventing Diseases
Vaccines are one of the most effective tools for preventing infectious diseases. They work by stimulating the immune system to recognize and combat pathogens, such as viruses or bacteria, without causing the disease itself. The success of vaccines in controlling diseases like smallpox, polio, and measles underscores their critical role in public health.
Myocarditis And Vaccines: The Current Evidence
COVID-19 Vaccines and Myocarditis
The association between COVID-19 vaccines and myocarditis has been a topic of extensive research and media coverage.
Reports of myocarditis following mRNA COVID-19 vaccinations (Pfizer-BioNTech and Moderna) have raised concerns, particularly among young males.
SEE ALSO: Can An Inflamed Heart Heal Itself?
Incidence Rates: Studies have shown that myocarditis following mRNA COVID-19 vaccination is rare. According to the Centers for Disease Control and Prevention (CDC), the incidence of myocarditis after mRNA vaccination is approximately 12.6 cases per million doses administered.
Demographic Variations: The risk is higher in males under 30 years of age, particularly after the second dose. However, the condition is generally mild and responds well to treatment.
Comparative Risk: It is important to note that the risk of myocarditis from COVID-19 infection itself is significantly higher than the risk associated with vaccination. A study published in the New England Journal of Medicine found that the risk of myocarditis was markedly higher following COVID-19 infection compared to vaccination.
Other Vaccines and Myocarditis
While the focus has been on COVID-19 vaccines, it is essential to consider the broader context of vaccines and myocarditis:
Smallpox Vaccine: Historically, the smallpox vaccine has been associated with myocarditis. The incidence is higher compared to mRNA COVID-19 vaccines, but the smallpox vaccine is no longer widely used following the eradication of the disease.
Influenza Vaccine: There is limited evidence to suggest a link between the influenza vaccine and myocarditis. Large-scale studies have not demonstrated a significant increase in myocarditis cases following influenza vaccination.
Other Vaccines: Vaccines such as those for measles, mumps, rubella, and hepatitis have not been conclusively linked to myocarditis. Reports of myocarditis following these vaccines are exceedingly rare and are typically within the background rate of myocarditis in the population.
Mechanisms Behind Vaccine-Associated Myocarditis
Understanding the potential mechanisms behind vaccine-associated myocarditis is critical for evaluating the risks and benefits:
Immune Response: Vaccines work by triggering an immune response, and in rare cases, this response may lead to inflammation of the heart muscle. The exact mechanism is not fully understood but may involve an overactive immune response.
Genetic Predisposition: Some individuals may have a genetic predisposition that makes them more susceptible to developing myocarditis following vaccination.
Molecular Mimicry: One hypothesis is that the immune system, in response to the vaccine, may produce antibodies that mistakenly attack the heart muscle, a phenomenon known as molecular mimicry.
Balancing The Risks And Benefits
When assessing the safety of vaccines, it is crucial to weigh the risks against the benefits. The risk of developing myocarditis following vaccination is low compared to the significant benefits of preventing severe disease, hospitalization, and death.
COVID-19 Vaccination: The benefits of COVID-19 vaccination in preventing severe illness, reducing transmission, and controlling the pandemic far outweigh the small risk of myocarditis.
Routine Vaccination: For routine childhood and adult vaccinations, the benefits in preventing potentially severe and life-threatening diseases greatly surpass the minimal risk of myocarditis.
Monitoring And Safety Measures
Public health agencies and regulatory bodies continually monitor the safety of vaccines through robust surveillance systems:
Vaccine Adverse Event Reporting System (VAERS): In the United States, VAERS allows for the reporting and analysis of adverse events following vaccination.
Clinical Trials and Post-Market Surveillance: Vaccines undergo rigorous testing in clinical trials before approval, and post-market surveillance ensures ongoing safety monitoring.
Public Communication: Transparent communication about the risks and benefits of vaccines is vital for maintaining public trust and ensuring informed decision-making.
Addressing Myths And Misinformation
Misinformation about vaccines and myocarditis can fuel vaccine hesitancy. Addressing common myths with evidence-based information is crucial:
Myth: All vaccines cause myocarditis.
Fact: Myocarditis is a rare side effect associated with a few vaccines, notably mRNA COVID-19 vaccines. Most vaccines have no significant link to myocarditis.
Myth: The risk of myocarditis from vaccines is higher than the risk from the diseases they prevent.
Fact: The risk of myocarditis from diseases like COVID-19 is substantially higher than from vaccination.
Conclusion
Do all vaccines cause myocarditis? The answer is a resounding no. While myocarditis has been observed as a rare side effect of certain vaccines, particularly mRNA COVID-19 vaccines, it is not a common outcome for most vaccines. The benefits of vaccination in preventing severe and potentially fatal diseases far outweigh the minimal risk of myocarditis. Ongoing research and surveillance continue to ensure vaccine safety and effectiveness, reinforcing the critical role of vaccines in public health.