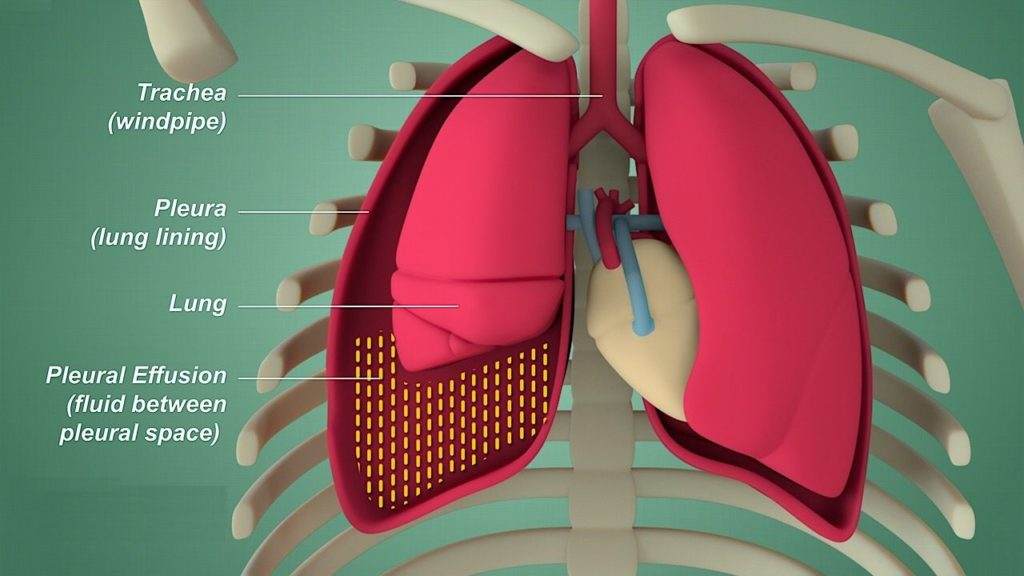
Heart failure is a complex cardiovascular condition that can have far-reaching effects on the body, including the development of pleural effusion. Pleural effusion refers to the abnormal accumulation of fluid in the pleural space, the thin membrane that surrounds the lungs. This condition can significantly impact a patient’s respiratory function and overall quality of life. In this article, we will delve into the mechanisms through which heart failure leads to pleural effusion, the clinical manifestations, diagnostic approaches, and management strategies.
How Heart Failure Causes Pleural Effusion
1. Pathophysiology of Heart Failure and Pleural Effusion
To comprehend how heart failure contributes to pleural effusion, it is essential to first understand the pathophysiology of heart failure itself. Heart failure occurs when the heart’s ability to pump blood efficiently is compromised, leading to inadequate perfusion of vital organs and tissues. This can result from various causes, including coronary artery disease, hypertension, valvular heart disease, or cardiomyopathy.
SEE ALSO: What Signs of Heart Problems in Newborns
In heart failure, the heart’s pumping mechanism is impaired, leading to a decrease in cardiac output. As a compensatory mechanism, the body activates neurohormonal pathways such as the renin-angiotensin-aldosterone system (RAAS) and the sympathetic nervous system (SNS) to maintain blood pressure and perfusion to vital organs. However, these compensatory mechanisms can also contribute to fluid retention and volume overload, which are central to the development of pleural effusion.
2. Fluid Dynamics in Heart Failure
In heart failure, the heart’s decreased pumping efficiency results in decreased forward flow of blood. This leads to increased pressure in the pulmonary veins and capillaries, a condition known as pulmonary congestion. The increased pressure in the pulmonary vasculature forces fluid (predominantly plasma) to leak into the interstitial spaces of the lungs, causing pulmonary edema.
As pulmonary edema progresses, the excess fluid can seep into the pleural space through small openings in the visceral pleura, the membrane covering the lungs. This fluid accumulation in the pleural space is termed pleural effusion. The fluid in pleural effusion is similar to the fluid in pulmonary edema, consisting of plasma with a high protein content and lacking red blood cells (transudative effusion).
Clinical Manifestations And Diagnosis
Patients with heart failure and pleural effusion may present with dyspnea (shortness of breath), especially on exertion or when lying flat (orthopnea). Other symptoms may include cough, fatigue, and lower extremity edema. Physical examination may reveal signs of fluid overload such as jugular venous distention, pulmonary crackles, and peripheral edema.
Diagnostic evaluation of heart failure and pleural effusion typically includes a thorough medical history, physical examination, chest X-ray, electrocardiogram (ECG), echocardiography, and laboratory tests such as brain natriuretic peptide (BNP) levels. Chest X-ray findings may show cardiomegaly (enlarged heart), pulmonary vascular congestion, and blunting of the costophrenic angles, indicative of pleural effusion.
Management Strategies
The management of heart failure with pleural effusion involves a multidisciplinary approach aimed at optimizing cardiac function, reducing fluid overload, and improving symptoms. Treatment strategies may include:
Medications: Diuretics such as furosemide (Lasix) are commonly used to reduce fluid retention and alleviate symptoms of congestion. ACE inhibitors, beta-blockers, aldosterone antagonists, and vasodilators may also be prescribed to improve cardiac function and reduce afterload.
Dietary Modifications: Patients with heart failure are often advised to follow a low-sodium diet to minimize fluid retention. Fluid restriction may also be recommended in severe cases.
Lifestyle Modifications: Encouraging physical activity within the patient’s functional capacity, smoking cessation, and weight management are integral components of heart failure management.
Monitoring: Regular follow-up visits with healthcare providers are essential to monitor the patient’s clinical status, adjust medications as needed, and assess for complications such as worsening heart failure or recurrent pleural effusion.
Interventional Procedures: In refractory cases or when conservative measures are insufficient, interventions such as thoracentesis (draining of pleural fluid), pleurodesis (inducing adhesion between pleural layers), or placement of a pleural drain may be considered.
Conclusion
Heart failure is a complex cardiovascular disorder that can lead to various complications, including pleural effusion.
Understanding the underlying pathophysiology of heart failure and its relationship to pleural effusion is crucial for effective management and improving patient outcomes. A comprehensive approach involving medical therapy, lifestyle modifications, and close monitoring is essential in optimizing the care of patients with heart failure and pleural effusion.