Coronary artery occlusion is a critical cardiovascular condition characterized by the blockage of one or more coronary arteries. These arteries are responsible for supplying oxygen-rich blood to the heart muscle. When they become obstructed, it can lead to significant cardiac issues, including myocardial infarction (heart attack) and other severe complications. To understand what causes coronary artery occlusion, it is essential to delve into the various factors and mechanisms that contribute to this life-threatening condition.
Atherosclerosis: The Primary Culprit
The Role of Atherosclerosis
Atherosclerosis is the most common cause of coronary artery occlusion. This condition involves the buildup of plaques within the arterial walls, composed mainly of lipids, cholesterol, calcium, and other substances found in the blood. Over time, these plaques can harden and narrow the arteries, reducing blood flow to the heart muscle.
see also: What Are The Treatment Options for Angiographic Obstruction
Development of Atherosclerotic Plaques
Atherosclerosis begins with endothelial dysfunction, where the inner lining of the arteries becomes damaged. Factors contributing to endothelial dysfunction include:
Hypertension (High Blood Pressure): Chronic high blood pressure can damage the arterial walls, making them more susceptible to plaque formation.
Hyperlipidemia (High Cholesterol Levels): Elevated levels of low-density lipoprotein (LDL) cholesterol contribute to plaque buildup.
Smoking: Chemicals in tobacco smoke can damage the endothelium and accelerate atherosclerosis.
Diabetes: High blood sugar levels can damage blood vessels and increase the risk of plaque formation.
Obesity: Excess body weight is associated with high blood pressure, diabetes, and abnormal lipid levels, all of which contribute to atherosclerosis.
Plaque Rupture and Thrombosis
The final step leading to coronary artery occlusion often involves plaque rupture. When a plaque ruptures, it exposes the underlying lipid core to the bloodstream, triggering the formation of a blood clot (thrombus). This clot can rapidly occlude the artery, cutting off blood supply to the heart muscle and causing a heart attack.
Other Causes of Coronary Artery Occlusion
Coronary Artery Spasm
Coronary artery spasm is a temporary, sudden narrowing of a coronary artery. It can significantly reduce or completely block blood flow. Factors that can trigger coronary artery spasm include:
Smoking: Nicotine and other chemicals in tobacco can induce spasms.
Drug Use: Cocaine and other illicit drugs can cause intense vasoconstriction.
Cold Exposure: Sudden exposure to cold can trigger coronary spasms in susceptible individuals.
Emotional Stress: Extreme emotional stress can lead to spasms of the coronary arteries.
Coronary Embolism
Coronary embolism is a less common cause of coronary artery occlusion. It occurs when a blood clot or other material (such as a fragment of atherosclerotic plaque or a tumor) travels through the bloodstream and lodges in a coronary artery.
Conditions that increase the risk of embolism include atrial fibrillation, infective endocarditis, and the presence of prosthetic heart valves.
Coronary Artery Dissection
Spontaneous coronary artery dissection (SCAD) is a rare condition where a tear forms in the coronary artery wall, creating a false lumen.
Blood can enter this false lumen, leading to the formation of a hematoma that compresses the true lumen and restricts blood flow.
SCAD is more common in women and can be associated with hormonal changes, connective tissue disorders, and intense physical or emotional stress.
Risk Factors for Coronary Artery Occlusion
Modifiable Risk Factors
Smoking: Smoking cessation significantly reduces the risk of coronary artery disease and occlusion.
Diet: A diet high in saturated fats, trans fats, and cholesterol can contribute to atherosclerosis. Adopting a heart-healthy diet rich in fruits, vegetables, whole grains, and lean proteins can mitigate this risk.
Physical Inactivity: Regular physical activity helps maintain healthy blood pressure, cholesterol levels, and body weight.
Obesity: Weight loss and maintenance of a healthy weight reduce the risk of diabetes, hypertension, and hyperlipidemia.
Alcohol Consumption: Excessive alcohol intake can lead to hypertension and contribute to atherosclerosis. Moderation is key.
Non-Modifiable Risk Factors
Age: The risk of coronary artery occlusion increases with age.
Gender: Men are at higher risk, but the risk for women increases and may equalize after menopause.
Family History: A family history of coronary artery disease increases an individual’s risk.
Genetics: Genetic factors can influence lipid metabolism, blood pressure regulation, and other mechanisms contributing to atherosclerosis.
Diagnostic Approaches
Clinical Evaluation
The diagnosis of coronary artery occlusion begins with a thorough clinical evaluation, including a detailed medical history and physical examination. Key symptoms suggesting occlusion include chest pain (angina), shortness of breath, fatigue, and palpitations.
Non-Invasive Tests
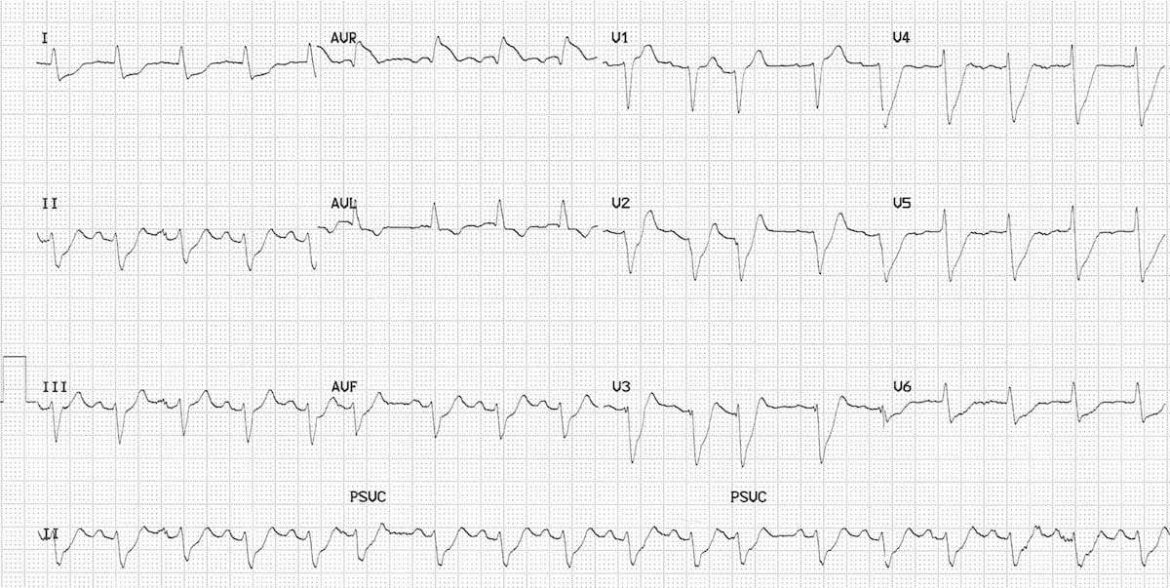
Electrocardiogram (ECG): An ECG can detect abnormalities in the heart’s electrical activity that suggest ischemia or infarction.
Stress Testing: Exercise or pharmacologic stress tests evaluate the heart’s response to increased workload and can identify areas of reduced blood flow.
Echocardiography: This ultrasound-based technique assesses heart function and structure, including wall motion abnormalities indicative of ischemia.
Cardiac CT: Coronary CT angiography provides detailed images of the coronary arteries and can detect the presence and severity of atherosclerotic plaques.
Invasive Tests
Coronary Angiography: This procedure involves injecting contrast dye into the coronary arteries via a catheter to visualize blockages directly.
It remains the gold standard for diagnosing coronary artery occlusion.
Treatment Strategies
Lifestyle Modifications
Smoking Cessation: Quitting smoking is paramount in reducing the risk of further occlusion.
Dietary Changes: Adopting a heart-healthy diet, such as the Mediterranean diet, can help manage lipid levels and reduce atherosclerosis progression.
Exercise: Regular physical activity improves cardiovascular health and reduces risk factors.
Weight Management: Achieving and maintaining a healthy weight through diet and exercise is crucial.
Medications
Antiplatelet Agents: Aspirin and other antiplatelet drugs prevent clot formation.
Statins: These medications lower cholesterol levels and stabilize plaques.
Beta-Blockers: They reduce the heart’s workload and oxygen demand.
ACE Inhibitors/ARBs: These drugs help manage blood pressure and reduce strain on the heart.
Calcium Channel Blockers: They can alleviate coronary artery spasms.
Interventional Procedures
Percutaneous Coronary Intervention (PCI): Also known as angioplasty, this procedure involves inflating a balloon within the blocked artery to restore blood flow. Often, a stent is placed to keep the artery open.
Coronary Artery Bypass Grafting (CABG): In severe cases, this surgical procedure creates new pathways for blood to flow around blocked arteries.
Prevention of Coronary Artery Occlusion
Primary Prevention
Preventing the initial occurrence of coronary artery occlusion involves addressing modifiable risk factors through lifestyle changes and medical management. Regular health screenings for blood pressure, cholesterol levels, and diabetes are essential.
Secondary Prevention
For individuals who have already experienced coronary artery occlusion, secondary prevention focuses on preventing recurrence.
This involves strict adherence to prescribed medications, lifestyle modifications, and regular follow-up with healthcare providers.
Conclusion
Coronary artery occlusion is a complex and multifaceted condition primarily caused by atherosclerosis, but also influenced by other factors such as coronary artery spasm, embolism, and dissection. Understanding the underlying mechanisms and risk factors is crucial for effective prevention, diagnosis, and treatment.