Transient idiopathic arrhythmia is a term used in cardiology to describe a type of irregular heart rhythm that occurs sporadically and without an identifiable cause. This condition is characterized by episodes of abnormal electrical activity in the heart, leading to irregular heartbeats or palpitations. While transient idiopathic arrhythmias are generally benign and self-limiting, understanding their nature, triggers, and management is crucial for patients and healthcare professionals alike.
What Is Arrhythmias?
Before delving into transient idiopathic arrhythmia, it’s essential to grasp the basics of arrhythmias in general. An arrhythmia refers to any abnormality in the rhythm or rate of the heartbeat. The heart’s electrical system controls the timing and sequence of heartbeats, ensuring efficient blood circulation throughout the body. When this electrical system malfunctions, arrhythmias can occur.
Arrhythmias are broadly classified into two categories based on their origin: supraventricular arrhythmias, which originate above the ventricles, and ventricular arrhythmias, which originate within the ventricles. Transient idiopathic arrhythmia falls under the category of supraventricular arrhythmias.
SEE ALSO: What Are The Causes And Symptoms of Atrial Flutter?
Characteristics of Transient Idiopathic Arrhythmia
Occurrence: Transient idiopathic arrhythmias are intermittent and may occur sporadically, making them challenging to predict or capture on standard electrocardiograms (ECGs).
Duration: These arrhythmias typically last for a short duration, ranging from seconds to minutes, and may resolve spontaneously without intervention.
Symptoms: Patients with transient idiopathic arrhythmias may experience palpitations, a feeling of fluttering or racing in the chest, dizziness, or lightheadedness during episodes. However, some individuals may be asymptomatic, and the arrhythmia may only be detected incidentally during medical evaluations.
Risk Factors: Unlike arrhythmias caused by structural heart disease or other identifiable triggers, transient idiopathic arrhythmias often occur in individuals without underlying heart conditions. However, factors such as stress, caffeine intake, alcohol consumption, and certain medications may trigger or exacerbate these arrhythmias in susceptible individuals.
Diagnosis And Evaluation
Diagnosing transient idiopathic arrhythmia requires a comprehensive evaluation, including:
Medical History: Understanding the patient’s medical history, symptoms, and potential triggers is essential in identifying transient idiopathic arrhythmias.
Physical Examination: A thorough physical examination, including assessment of heart sounds, blood pressure, and signs of cardiovascular disease, helps rule out other cardiac conditions.
Electrocardiogram (ECG): While transient idiopathic arrhythmias may not always be captured on a standard ECG due to their sporadic nature, continuous monitoring devices such as Holter monitors or event recorders may be used to capture episodes over an extended period.
Laboratory Tests: Blood tests may be conducted to assess electrolyte levels, thyroid function, and other metabolic parameters that can influence cardiac rhythm.
Imaging Studies: In some cases, imaging studies such as echocardiography or cardiac MRI may be performed to evaluate the heart’s structure and function.
Management And Treatment
The management of transient idiopathic arrhythmia focuses on:
Lifestyle Modifications: Patients are advised to make lifestyle changes to minimize arrhythmia triggers. This may include reducing caffeine and alcohol intake, managing stress through relaxation techniques or counseling, and maintaining a healthy diet and regular exercise routine.
Medication: In certain cases, medications such as beta-blockers or calcium channel blockers may be prescribed to help control heart rate and rhythm during arrhythmic episodes. However, the use of medications depends on the individual’s overall health and the frequency and severity of arrhythmias.
Monitoring: Regular follow-up appointments and periodic monitoring with ambulatory ECG devices may be recommended to track arrhythmia patterns and assess treatment efficacy.
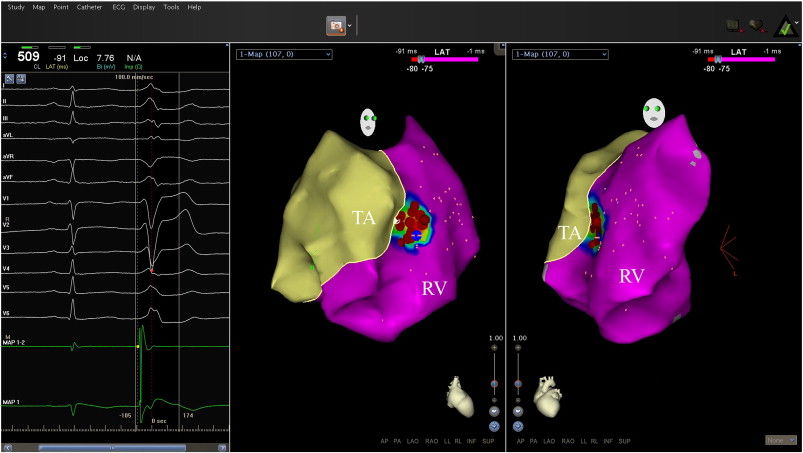
Electrophysiology Studies: In cases where the underlying cause of transient idiopathic arrhythmia is unclear or if the arrhythmias are recurrent and symptomatic, electrophysiology studies may be performed to identify specific electrical abnormalities in the heart’s conduction system.
Prognosis And Outlook
The prognosis for individuals with transient idiopathic arrhythmia is generally favorable, with most patients experiencing infrequent and benign episodes. By identifying and avoiding potential triggers, adhering to medication regimens if prescribed, and maintaining regular follow-up with healthcare providers, individuals with transient idiopathic arrhythmia can effectively manage their condition and lead healthy, active lives.
Conclution
In conclusion, transient idiopathic arrhythmia represents a subset of supraventricular arrhythmias characterized by intermittent episodes of irregular heart rhythm without an identifiable cause. While typically benign, proper diagnosis, evaluation, and management are essential in ensuring optimal outcomes for affected individuals. Collaborative efforts between patients, healthcare providers, and cardiologists play a crucial role in addressing transient idiopathic arrhythmia and promoting cardiovascular health.