Cardiogenic shock and heart failure are two critical conditions related to the heart, yet they differ significantly in their mechanisms, severity, and management. Understanding these differences is crucial for healthcare professionals and patients alike to ensure accurate diagnosis, appropriate treatment, and improved outcomes.
Cardiogenic Shock: A Life-Threatening Emergency
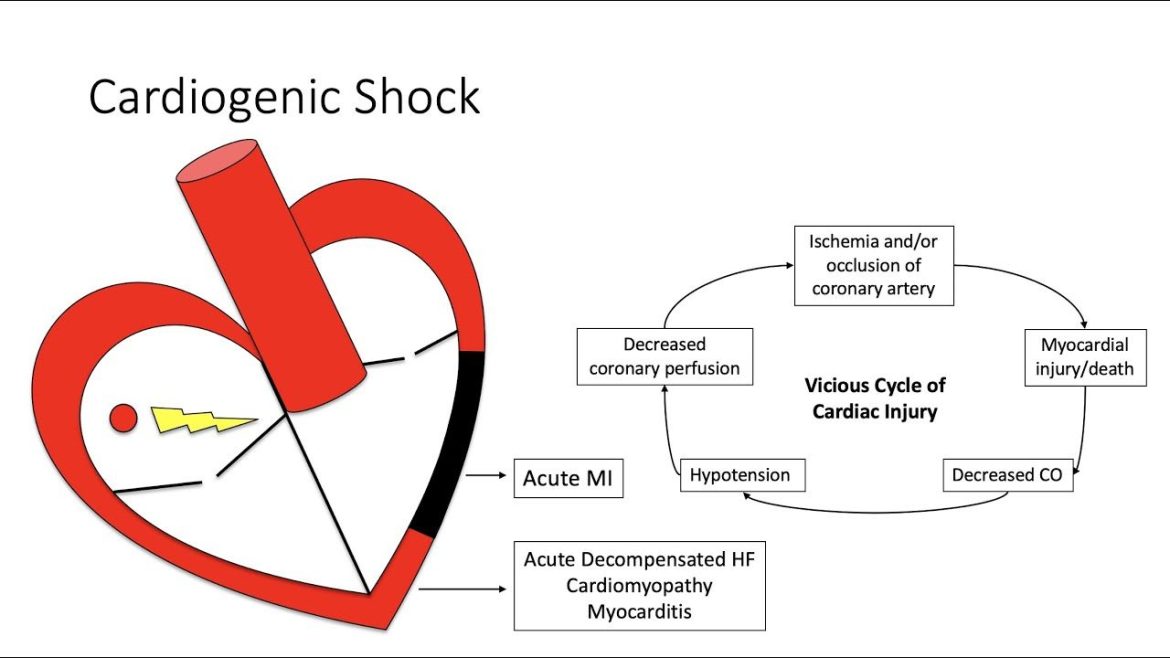
Cardiogenic shock is a severe condition characterized by inadequate tissue perfusion due to the heart’s inability to pump effectively. It often arises as a complication of various cardiac events, such as myocardial infarction (heart attack), severe arrhythmias, or acute decompensation of pre-existing heart failure. In cardiogenic shock, the heart’s pumping function is severely compromised, leading to systemic hypoperfusion and organ dysfunction.
The hallmark of cardiogenic shock is profound hemodynamic instability, including hypotension (low blood pressure), tachycardia (rapid heart rate), and signs of end-organ damage such as altered mental status, cool extremities, and oliguria (decreased urine output).
Immediate intervention is paramount in cardiogenic shock, typically involving aggressive fluid resuscitation, inotropic support to enhance heart contractility, vasopressors to maintain blood pressure, and mechanical circulatory support devices like intra-aortic balloon pumps or extracorporeal membrane oxygenation (ECMO).
see also: What Causes Decreased Heart Function?
Heart Failure: A Chronic Condition with Acute Exacerbations
Heart failure, on the other hand, is a chronic progressive condition where the heart’s ability to pump blood efficiently is compromised over time. It can result from various underlying causes, including coronary artery disease, hypertension, valvular heart disease, or cardiomyopathies. Heart failure is categorized based on ejection fraction into heart failure with reduced ejection fraction (HFrEF) and heart failure with preserved ejection fraction (HFpEF).
Unlike cardiogenic shock, heart failure typically presents with a constellation of symptoms that may include dyspnea (shortness of breath), fatigue, exercise intolerance, peripheral edema, and fluid retention. While heart failure can lead to acute decompensation episodes requiring hospitalization, it often follows a more predictable course with periods of stability interspersed with exacerbations.
Management of heart failure involves lifestyle modifications, pharmacological therapy including ACE inhibitors, beta-blockers, diuretics, and in select cases, device therapy such as implantable cardioverter-defibrillators (ICDs) or cardiac resynchronization therapy (CRT). Cardiac rehabilitation, dietary adjustments, and close monitoring of fluid balance and symptoms are integral parts of heart failure management.
Key Differences And Similarities
The fundamental difference between cardiogenic shock and heart failure lies in their acuity and severity. Cardiogenic shock is an acute, life-threatening condition requiring immediate intervention to stabilize hemodynamics and prevent organ failure. In contrast, heart failure is a chronic condition that may manifest acutely during exacerbations but generally follows a more predictable course.
Another crucial distinction is the degree of cardiac dysfunction. In cardiogenic shock, the heart’s pumping function is severely impaired, often leading to multiorgan failure if not promptly addressed. In heart failure, while cardiac function is compromised, it is typically not to the extent seen in cardiogenic shock.
However, it’s important to note that cardiogenic shock can be a complication of heart failure, particularly during acute decompensation episodes. In such cases, the underlying heart failure exacerbation may precipitate cardiogenic shock, necessitating aggressive management to restore cardiac output and perfusion.
Conclusion
In summary, cardiogenic shock and heart failure are distinct yet interconnected conditions related to cardiac dysfunction. While cardiogenic shock represents a severe, acute state of inadequate tissue perfusion due to compromised cardiac function, heart failure is a chronic condition characterized by ongoing impairment in cardiac performance. Understanding the differences between these conditions is vital for healthcare providers to deliver timely and appropriate interventions, ultimately improving patient outcomes and quality of life.
FAQs
Is heart failure the same as cardiogenic shock?
No, heart failure and cardiogenic shock are not the same. Heart failure is a chronic condition where the heart’s ability to pump blood efficiently is compromised over time. Cardiogenic shock, on the other hand, is an acute and life-threatening condition where the heart’s pumping function is severely impaired, leading to inadequate tissue perfusion.
What is cardiogenic shock acute heart failure?
Cardiogenic shock is a condition of acute circulatory failure due to the heart’s inability to pump effectively. It can be a complication of various cardiac events, inc
luding acute exacerbations of heart failure, myocardial infarction (heart attack), or severe arrhythmias. Acute heart failure refers to a sudden onset or worsening of heart failure symptoms, which may or may not progress to cardiogenic shock depending on the severity and underlying causes.
Is cardiogenic shock pump failure?
Yes, cardiogenic shock can be described as pump failure because it involves the heart’s inability to pump blood effectively to meet the body’s demands. This pump failure leads to systemic hypoperfusion and organ dysfunction, necessitating immediate intervention to stabilize hemodynamics and restore cardiac function.