Heart failure, a condition characterized by the heart’s inability to pump blood effectively, affects millions of people worldwide and is a significant cause of morbidity and mortality. While it can occur in individuals of any age and gender, there has been ongoing research and debate about whether heart failure is more prevalent in men or women.
Understanding the gender differences in heart failure incidence, risk factors, presentation, and outcomes is crucial for effective management and prevention strategies.
Incidence And Prevalence
Historically, heart failure has been considered more common in men. However, recent studies have highlighted significant gender-related differences in heart failure epidemiology. According to the American Heart Association (AHA), heart failure affects approximately 6.2 million adults in the United States, with a slightly higher prevalence in men than women.
However, when considering specific age groups, the prevalence of heart failure in women increases with advancing age, particularly after menopause.
see also: Cardiogenic Shock Vs Heart Failure: What Is The Same?
Risk Factors
Several risk factors contribute to the development of heart failure, and their prevalence varies between men and women.
For instance, coronary artery disease (CAD) and myocardial infarction (MI) are more prevalent in men, leading to a higher incidence of heart failure secondary to ischemic heart disease. On the other hand, women are more likely to develop heart failure due to hypertension, valvular heart disease, and cardiomyopathies such as dilated cardiomyopathy (DCM) and peripartum cardiomyopathy (PPCM).
Pathophysiology And Presentation
The pathophysiological mechanisms underlying heart failure also exhibit gender-specific differences. Men tend to develop heart failure with reduced ejection fraction (HFrEF), characterized by impaired contractility of the heart muscle. In contrast, women are more likely to present with heart failure with preserved ejection fraction (HFpEF), where the heart’s pumping function is preserved, but there is impaired relaxation or stiffness of the ventricles.
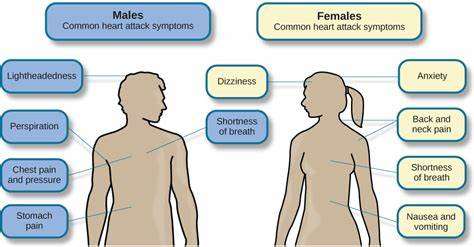
The clinical presentation of heart failure can also vary between men and women. Men often present with classic symptoms such as exertional dyspnea, fatigue, and peripheral edema. In contrast, women may experience more atypical symptoms such as shortness of breath at rest, fatigue, and palpitations, which can lead to underdiagnosis or delayed diagnosis of heart failure in women.
Outcomes And Prognosis
Studies evaluating the outcomes and prognosis of heart failure have reported mixed findings regarding gender differences.
While some studies suggest that men have a higher risk of heart failure-related mortality, others indicate that women may have worse outcomes post-heart failure diagnosis, including higher rates of hospitalization and readmission. These variations in outcomes may be attributed to differences in age, comorbidities, response to treatment, and access to healthcare services.
Treatment And Management
The management of heart failure involves a multidisciplinary approach focusing on lifestyle modifications, pharmacological interventions, device therapy, and, in some cases, surgical interventions such as heart transplantation. Tailoring treatment strategies based on gender-specific differences in etiology, symptomatology, and response to therapy is essential for optimizing outcomes in patients with heart failure.
Conclusion
In conclusion, the question of whether heart failure is more common in men or women is multifaceted and influenced by various factors including age, risk factors, pathophysiology, presentation, outcomes, and treatment response. While men traditionally exhibit a higher prevalence of heart failure, gender-specific differences in risk factors, clinical profiles, and outcomes highlight the need for personalized and gender-tailored approaches to the prevention, diagnosis, and management of heart failure.
Further research and awareness are necessary to address the complexities of gender disparities in heart failure and improve cardiovascular health outcomes for all individuals.
FAQs
Who is most likely to get heart failure?
Heart failure can affect individuals of all ages, genders, and ethnicities. However, certain factors increase the likelihood of developing heart failure, including older age, a history of heart disease (such as coronary artery disease or heart attack), high blood pressure, diabetes, obesity, and a family history of heart failure.
Who has more heart disease, male or female?
Historically, men have had a higher prevalence of heart disease, including conditions like coronary artery disease (CAD) and heart failure. However, the incidence of heart disease in women has been increasing, particularly after menopause. Women also tend to develop heart disease later in life compared to men.
What population is more prone to heart failure?
Several populations are more prone to heart failure, including individuals with a history of heart disease, high blood pressure, diabetes, obesity, chronic kidney disease, and certain ethnic groups such as African Americans and Hispanics.
Aging is also a significant risk factor for heart failure.