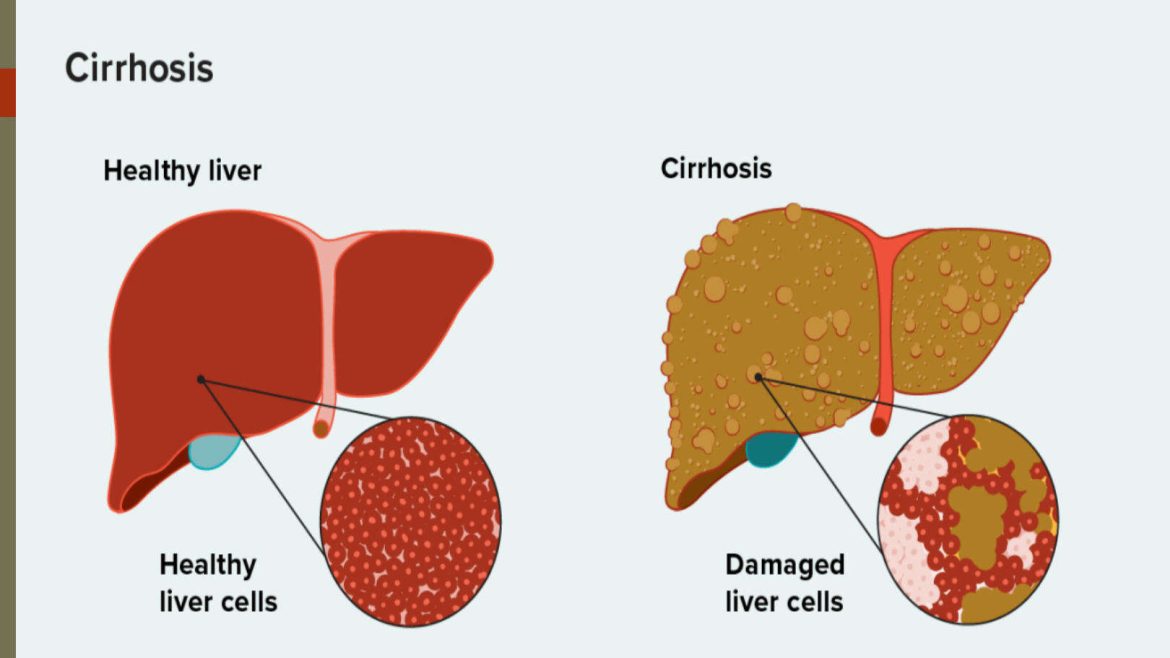
Portal hypertension is a significant clinical condition often associated with cirrhosis, a chronic liver disease characterized by the replacement of healthy liver tissue with scar tissue. This article aims to provide a comprehensive understanding of portal hypertension in cirrhosis, covering its pathophysiology, causes, symptoms, complications, diagnostic methods, and treatment options.
Pathophysiology of Portal Hypertension
Portal hypertension occurs when there is an increase in the blood pressure within the portal venous system, which comprises the portal vein and its branches. The portal vein is responsible for carrying blood from the gastrointestinal organs to the liver. In cirrhosis, the formation of scar tissue disrupts the normal architecture of the liver, leading to increased resistance to blood flow through the liver. This resistance causes a backlog of blood, resulting in increased pressure within the portal vein.
SEE ALSO: What Causes Super High Blood Pressure?
Causes of Portal Hypertension in Cirrhosis
The primary cause of portal hypertension in cirrhosis is the scarring of liver tissue, which can result from various liver diseases and conditions, including:
Chronic Hepatitis B and C Infections: Persistent viral infections can lead to liver inflammation and scarring over time.
Alcoholic Liver Disease: Chronic alcohol abuse causes liver damage and cirrhosis.
Non-Alcoholic Steatohepatitis (NASH): This condition, related to obesity and metabolic syndrome, leads to liver inflammation and fibrosis.
Autoimmune Hepatitis: An autoimmune disorder where the body’s immune system attacks liver cells.
Primary Biliary Cholangitis and Primary Sclerosing Cholangitis: Chronic liver diseases affecting the bile ducts, leading to cirrhosis.
Genetic Disorders: Conditions like hemochromatosis and Wilson’s disease can cause liver damage and cirrhosis.
Symptoms of Portal Hypertension
The symptoms of portal hypertension are often related to its complications rather than the condition itself. Common symptoms include:
Ascites: Accumulation of fluid in the abdominal cavity, leading to swelling and discomfort.
Variceal Bleeding: Enlarged veins (varices) in the esophagus or stomach that can rupture and cause severe bleeding.
Splenomegaly: Enlargement of the spleen due to increased pressure in the splenic vein, which is part of the portal system.
Hepatic Encephalopathy: Mental confusion and other neurological symptoms resulting from toxins that the damaged liver cannot process.
Jaundice: Yellowing of the skin and eyes due to the buildup of bilirubin.
Complications of Portal Hypertension
Portal hypertension can lead to several life-threatening complications, including:
Variceal Hemorrhage: One of the most severe complications, where ruptured varices cause massive gastrointestinal bleeding, leading to shock and potentially death if not promptly treated.
Ascites: Severe ascites can cause discomfort, respiratory issues, and an increased risk of bacterial infections like spontaneous bacterial peritonitis (SBP).
Hepatorenal Syndrome: A type of kidney failure that occurs in patients with severe liver disease.
Portal Hypertensive Gastropathy: Changes in the stomach lining due to high portal pressure, leading to bleeding.
Hepatopulmonary Syndrome: A condition where abnormal blood vessels form in the lungs, causing oxygenation issues.
Diagnosis of Portal Hypertension
Diagnosing portal hypertension involves a combination of clinical evaluation, imaging studies, and sometimes invasive procedures:
Clinical Evaluation: A thorough history and physical examination to identify symptoms and signs of portal hypertension.
Laboratory Tests: Blood tests to assess liver function and detect complications like variceal bleeding or renal impairment.
Imaging Studies: Ultrasound, CT scan, and MRI can visualize the liver, portal vein, and detect complications such as ascites and splenomegaly.
Endoscopy: Esophagogastroduodenoscopy (EGD) is used to identify and monitor varices in the esophagus and stomach.
Hepatic Venous Pressure Gradient (HVPG) Measurement: An invasive procedure to measure the pressure gradient between the portal vein and hepatic veins, which is the gold standard for diagnosing portal hypertension.
Treatment of Portal Hypertension
Treatment of portal hypertension focuses on managing the underlying cirrhosis, preventing complications, and addressing specific symptoms. The main strategies include:
Medical Therapy:
Beta-Blockers: Non-selective beta-blockers like propranolol and nadolol reduce portal pressure and the risk of variceal bleeding.
Diuretics: Medications like spironolactone and furosemide are used to manage ascites by reducing fluid accumulation.
Lactulose and Rifaximin: These are used to manage hepatic encephalopathy by reducing ammonia levels in the blood.
Endoscopic Therapy:
Endoscopic Variceal Ligation (EVL): A procedure to band varices and prevent bleeding.
Sclerotherapy: Injection of a sclerosing agentinto varices to obliterate them.
Interventional Radiology:
Transjugular Intrahepatic Portosystemic Shunt (TIPS): A procedure to create a pathway between the portal vein and hepatic vein, reducing portal pressure.
Paracentesis: A procedure to drain ascitic fluid from the abdominal cavity.
Surgery:
Liver Transplantation: The definitive treatment for patients with end-stage liver disease and refractory portal hypertension. It involves replacing the damaged liver with a healthy donor liver.
Prevention And Lifestyle Modifications
Preventing the progression of liver disease and managing portal hypertension involves several lifestyle changes and preventive measures:
Alcohol Abstinence: Avoiding alcohol to prevent further liver damage.
Healthy Diet: Eating a balanced diet with adequate protein and low sodium to manage ascites and overall health.
Regular Monitoring: Routine follow-ups with a healthcare provider to monitor liver function and detect complications early.
Vaccinations: Ensuring vaccination against hepatitis A and B to prevent superimposed infections.
Conclusion
Portal hypertension in cirrhosis is a complex condition with significant clinical implications. Understanding its pathophysiology, causes, symptoms, complications, and treatment options is crucial for effective management. Early diagnosis and intervention, along with lifestyle modifications, can improve the quality of life and outcomes for patients with cirrhosis and portal hypertension. As advancements in medical research continue, new therapeutic approaches and better management strategies will likely emerge, offering hope for better prognosis and improved patient care.