Fluid overload, also known as hypervolemia, is a common and critical complication in patients with heart failure. It occurs when the heart is unable to pump blood effectively, leading to a buildup of fluid in the body’s tissues. Recognizing the signs and symptoms of fluid overload is essential for early intervention and management, which can significantly improve the quality of life and outcomes for patients with heart failure. In this article, we will explore the various signs and symptoms of fluid overload in heart failure, the underlying mechanisms, and the importance of timely diagnosis and treatment.
What Is Fluid Overload?
Fluid overload refers to an excessive accumulation of fluid in the body’s tissues and cavities. In the context of heart failure, it results from the heart’s inability to pump blood efficiently, causing blood to back up into the veins and leading to fluid leakage into the tissues. This condition can affect various parts of the body, including the lungs, abdomen, and extremities.
Mechanisms of Fluid Overload in Heart Failure
Heart failure can be classified into two main types: systolic and diastolic. Systolic heart failure occurs when the heart’s pumping function is weakened, while diastolic heart failure involves a stiffening of the heart muscle, which impairs its ability to relax and fill with blood. Both types can lead to fluid overload through different mechanisms.
Systolic Heart Failure: The reduced ejection fraction in systolic heart failure means the heart cannot pump out enough blood with each beat, leading to blood pooling in the ventricles. This causes an increase in pressure within the heart chambers, which eventually forces fluid out of the blood vessels and into the surrounding tissues.
Diastolic Heart Failure: In diastolic heart failure, the heart muscle becomes stiff and less compliant, making it difficult for the ventricles to fill with blood. This results in increased pressure in the atria and pulmonary veins, leading to fluid leakage into the lungs and other tissues.
SEE ALSO: Is Heart Disease A Genetic Disorder?
Signs And Symptoms of Fluid Overload in Heart Failure
Fluid overload can manifest in various ways, depending on the severity and location of fluid accumulation. The following are some of the most common signs and symptoms associated with fluid overload in heart failure:
Peripheral Edema
Peripheral edema, or swelling in the extremities, is one of the hallmark signs of fluid overload in heart failure. It typically starts in the feet and ankles and can progress to the legs and thighs. Patients may notice that their shoes feel tighter, and they may have difficulty wearing socks or shoes that previously fit comfortably.
Characteristics of Peripheral Edema
Pitting Edema: When pressure is applied to the swollen area, it leaves an indentation or “pit” that persists for some time.
This is a classic sign of fluid accumulation.
Bilateral Swelling: Edema in heart failure usually affects both legs, although one side may be more pronounced.
Progressive Nature: The swelling often worsens as the day goes on, especially after prolonged periods of sitting or standing.
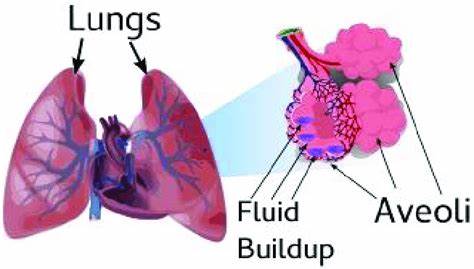
Pulmonary Edema
Pulmonary edema occurs when fluid accumulates in the lungs, making it difficult for patients to breathe. This is a serious condition that requires immediate medical attention.
Symptoms of Pulmonary Edema
Dyspnea (Shortness of Breath): Patients may experience difficulty breathing, particularly when lying flat (orthopnea) or during physical activity.
Paroxysmal Nocturnal Dyspnea (PND): Sudden episodes of severe shortness of breath that wake patients from sleep.
Coughing: A persistent cough, which may produce frothy or pink-tinged sputum.
Wheezing: A high-pitched whistling sound during breathing, indicating fluid in the airways.
Ascites
Ascites is the accumulation of fluid in the abdominal cavity, which can cause noticeable swelling and discomfort. This symptom is more common in advanced stages of heart failure.
Characteristics of Ascites
Abdominal Distension: A visible increase in abdominal girth, often accompanied by a feeling of fullness or tightness.
Weight Gain: Rapid and unexplained weight gain due to fluid retention.
Discomfort and Pain: Patients may experience discomfort, bloating, and sometimes pain in the abdomen.
Jugular Venous Distention (JVD)
Jugular venous distention is the visible bulging of the jugular veins in the neck, which indicates increased pressure in the right atrium and venous system.
Signs of JVD
Elevated Jugular Venous Pressure (JVP): Measurement of JVP can provide valuable information about fluid status and cardiac function.
Prominent Neck Veins: The jugular veins may appear visibly distended, especially when the patient is seated or reclined at a 45-degree angle.
Rapid Weight Gain
Rapid and unexplained weight gain is a common indicator of fluid retention. Patients with heart failure are often advised to monitor their weight daily to detect sudden increases.
Factors Contributing to Weight Gain
Fluid Retention: Accumulation of fluid in the tissues can lead to significant weight gain over a short period.
Decreased Urine Output: Reduced kidney function in heart failure can result in decreased urine production and fluid retention.
Fatigue and Weakness
Fluid overload can cause reduced oxygen delivery to the tissues, leading to fatigue and general weakness. This can significantly impact a patient’s ability to perform daily activities and reduce their quality of life.
Symptoms of Fatigue and Weakness
Exercise Intolerance: Difficulty engaging in physical activities that were previously manageable.
Muscle Weakness: Generalized weakness, particularly in the legs and arms.
Decreased Appetite and Nausea
Fluid accumulation in the abdomen can compress the stomach and intestines, leading to decreased appetite, early satiety, and sometimes nausea.
Gastrointestinal Symptoms
Loss of Appetite: Reduced desire to eat, often accompanied by a feeling of fullness after eating small amounts.
Nausea and Vomiting: In severe cases, patients may experience nausea and occasional vomiting.
Importance of Timely Diagnosis And Treatment
Early recognition and management of fluid overload in heart failure are crucial to prevent complications and improve patient outcomes. Timely intervention can help reduce the burden on the heart, alleviate symptoms, and enhance the overall quality of life.
Diagnostic Tools
Physical Examination: Assessment of peripheral edema, JVD, and other signs of fluid overload.
Imaging Studies: Chest X-rays and echocardiograms can help visualize fluid accumulation in the lungs and heart.
Laboratory Tests: Blood tests to evaluate kidney function, electrolyte levels, and markers of heart failure such as B-type natriuretic peptide (BNP).
Treatment Strategies
Diuretics: Medications that help remove excess fluid from the body by increasing urine output.
Lifestyle Modifications: Dietary changes, such as reducing sodium intake and limiting fluid consumption, can help manage fluid overload.
Monitoring and Follow-up: Regular monitoring of weight, symptoms, and laboratory parameters to detect and address fluid retention promptly.
Conclusion
Fluid overload is a significant and common complication in patients with heart failure. Recognizing the signs and symptoms of fluid overload, such as peripheral edema, pulmonary edema, ascites, jugular venous distention, rapid weight gain, fatigue, and gastrointestinal symptoms, is essential for early diagnosis and effective management. Timely intervention can help alleviate symptoms, prevent complications, and improve the quality of life for individuals living with heart failure.