Atherosclerosis of the native coronary artery is a specific type of cardiovascular disease that affects the arteries supplying blood to the heart muscle. This condition is characterized by the accumulation of plaque within the arterial walls, leading to narrowed or blocked arteries. This article explores the definition, causes, symptoms, diagnosis, treatment, and prevention of atherosclerosis of the native coronary artery, providing a comprehensive overview for better understanding and management.
Definition And Mechanism
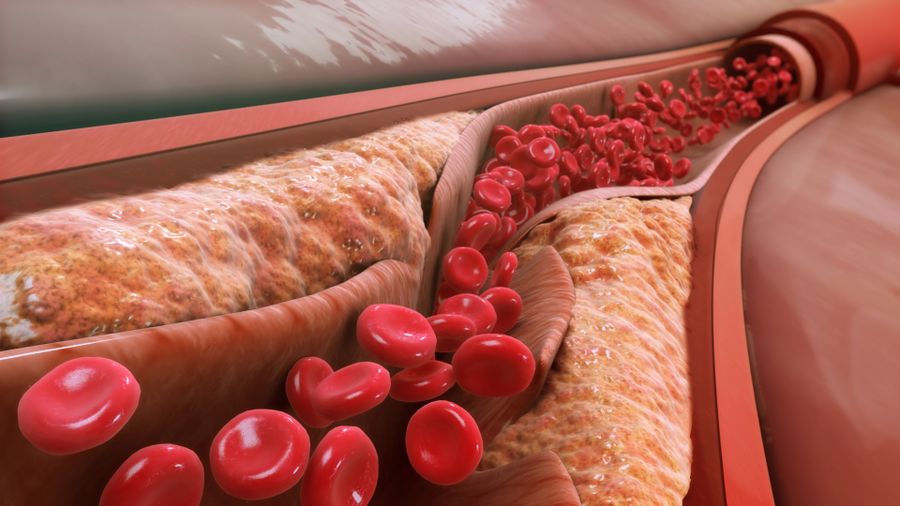
Atherosclerosis is a chronic, progressive disease characterized by the buildup of plaque—a mixture of fatty deposits, cholesterol, calcium, and other substances—within the inner walls of arteries. When this process occurs in the coronary arteries, which supply oxygen-rich blood to the heart muscle, it is referred to as atherosclerosis of the native coronary artery.
SEE ALSO: 3 Risk Factors for Coronary Artery Disease
Plaque Formation
The formation of plaque in the arteries is a complex process that begins with endothelial injury. The endothelium is a thin layer of cells lining the arteries, and it can be damaged by factors such as high blood pressure, smoking, high cholesterol, and diabetes. Once the endothelium is damaged, low-density lipoprotein (LDL) cholesterol penetrates the arterial wall and becomes oxidized. This triggers an inflammatory response, attracting white blood cells (macrophages) to the site of injury.
Foam Cells And Fatty Streaks
Macrophages engulf oxidized LDL cholesterol, transforming into foam cells. These foam cells accumulate to form fatty streaks, the earliest visible form of atherosclerotic lesions. Over time, smooth muscle cells migrate to the intima (inner layer of the artery) and proliferate, producing extracellular matrix components that form a fibrous cap over the plaque. This process results in the development of a more advanced and complex plaque structure.
Plaque Stability And Rupture
Plaques can vary in stability. Stable plaques have a thick fibrous cap and are less likely to rupture, while unstable plaques have a thin fibrous cap and a large lipid core, making them prone to rupture. Plaque rupture can lead to the formation of a blood clot (thrombus) that partially or completely occludes the artery, potentially causing a heart attack (myocardial infarction).
Causes And Risk Factors
Atherosclerosis of the native coronary artery is influenced by several modifiable and non-modifiable risk factors.
Non-modifiable Risk Factors
Age: The risk of atherosclerosis increases with age.
Gender: Men are at higher risk of developing atherosclerosis at an earlier age than women.
Family History: A family history of heart disease increases the risk.
Modifiable Risk Factors
High Blood Pressure (Hypertension): Increased pressure on arterial walls can damage the endothelium.
High Cholesterol Levels: Elevated levels of LDL cholesterol contribute to plaque formation.
Smoking: Smoking damages the endothelium and promotes atherosclerosis.
Diabetes: High blood sugar levels can damage blood vessels and promote plaque buildup.
Obesity: Excess weight is associated with other risk factors like hypertension and diabetes.
Sedentary Lifestyle: Lack of physical activity contributes to obesity and other risk factors.
Unhealthy Diet: Diets high in saturated fats, trans fats, and cholesterol can raise blood cholesterol levels.
Excessive Alcohol Consumption: High alcohol intake can raise blood pressure and cholesterol levels.
Symptoms And Complications
Angina Pectoris
One of the most common symptoms of atherosclerosis of the native coronary artery is angina pectoris, or chest pain.
Angina is often described as a pressure or squeezing sensation in the chest, and it can radiate to the shoulders, arms, neck, jaw, or back. Angina occurs when the heart muscle does not receive enough oxygen-rich blood, particularly during physical exertion or emotional stress.
Shortness of Breath
Atherosclerosis can also cause shortness of breath, especially during physical activity. This symptom occurs because the heart is not receiving enough oxygenated blood to meet the increased demands of the body.
Heart Attack (Myocardial Infarction)
A heart attack occurs when a coronary artery becomes completely blocked, usually by a blood clot that forms on a ruptured plaque. This blockage prevents oxygen-rich blood from reaching a portion of the heart muscle, causing the tissue to become damaged or die.
Symptoms of a heart attack include intense chest pain or discomfort, shortness of breath, nausea, vomiting, and sweating.
Heart Failure
Chronic atherosclerosis can weaken the heart muscle over time, leading to heart failure. In heart failure, the heart cannot pump blood effectively to meet the body’s needs, resulting in symptoms such as fatigue, shortness of breath, and swelling in the legs and ankles.
Arrhythmias
Atherosclerosis can also lead to arrhythmias, or irregular heartbeats. These can range from harmless to life-threatening and may cause palpitations, dizziness, fainting, or sudden cardiac arrest.
Diagnosis
Medical History and Physical Examination
Diagnosis begins with a thorough medical history and physical examination. The healthcare provider will inquire about symptoms, risk factors, and family history of heart disease. During the physical examination, they may listen for abnormal heart sounds or check for signs of poor circulation.
Electrocardiogram (ECG or EKG)
An electrocardiogram records the electrical activity of the heart and can detect abnormalities that suggest atherosclerosis, such as changes in heart rhythm or evidence of a previous heart attack.
Stress Testing
Stress testing evaluates the heart’s function during physical exertion.
Patients may walk on a treadmill or ride a stationary bike while their heart rate, blood pressure, and ECG are monitored.
Stress tests can reveal symptoms of atherosclerosis, such as angina, that occur during exercise.
Echocardiogram
An echocardiogram uses ultrasound waves to create images of the heart. It can assess the size, shape, and function of the heart, as well as the movement of blood through the chambers and valves.
Coronary Angiography
Coronary angiography is an invasive test that provides detailed images of the coronary arteries. A contrast dye is injected into the bloodstream, and X-ray images are taken to identify areas of narrowing or blockage. This procedure is often performed in conjunction with cardiac catheterization.
Blood Tests
Blood tests can measure levels of cholesterol, triglycerides, blood sugar, and other markers that indicate an increased risk of atherosclerosis.
Treatment
Lifestyle Changes
Healthy Diet: Adopting a diet low in saturated fats, trans fats, cholesterol, and sodium can help reduce plaque buildup.
Emphasize fruits, vegetables, whole grains, lean proteins, and healthy fats.
Regular Exercise: Physical activity can improve cardiovascular health, reduce weight, and lower blood pressure and cholesterol levels.
Smoking Cessation: Quitting smoking can significantly reduce the risk of atherosclerosis and improve overall health.
Weight Management: Maintaining a healthy weight can lower the risk of atherosclerosis and related conditions.
Moderate Alcohol Consumption: Limiting alcohol intake can help control blood pressure and cholesterol levels.
Medications
Statins: Statins are commonly prescribed to lower LDL cholesterol levels and reduce plaque formation.
Antihypertensive Medications: Medications such as beta-blockers, ACE inhibitors, and calcium channel blockers can help control high blood pressure.
Antiplatelet Agents: Aspirin and other antiplatelet drugs can reduce the risk of blood clot formation.
Diabetes Medications: Proper management of diabetes can help prevent complications related to atherosclerosis.
Surgical and Interventional Procedures
Angioplasty and Stenting: During angioplasty, a balloon catheter is inserted into the narrowed artery and inflated to widen it. A stent (a small mesh tube) is then placed to keep the artery open.
Coronary Artery Bypass Grafting (CABG): In CABG surgery, a healthy blood vessel from another part of the body is used to bypass the blocked artery, creating a new pathway for blood flow to the heart muscle.
Prevention
Regular Health Screenings
Routine check-ups and screenings can detect early signs of atherosclerosis and other cardiovascular diseases. Monitoring blood pressure, cholesterol levels, and blood sugar levels is crucial for early intervention.
Healthy Lifestyle Choices
Adopting and maintaining a healthy lifestyle can significantly reduce the risk of atherosclerosis. This includes eating a balanced diet, engaging in regular physical activity, avoiding smoking, and limiting alcohol consumption.
Managing Chronic Conditions
Proper management of chronic conditions such as hypertension, diabetes, and high cholesterol is essential in preventing the progression of atherosclerosis. Follow your healthcare provider’s recommendations for medications, lifestyle changes, and monitoring.
Conclusion
Atherosclerosis of the native coronary artery is a serious condition that can lead to life-threatening complications such as heart attack, heart failure, and arrhythmias. Understanding the risk factors, symptoms, and treatment options is crucial for managing this condition effectively. Through lifestyle changes, medications, and medical procedures, individuals can reduce their risk and improve their cardiovascular health. Regular health screenings and proactive management of chronic conditions are key components in preventing and controlling atherosclerosis of the native coronary artery.