In recent years, the medical community has been consistently focused on refining guidelines to manage and reduce the risk of cardiovascular diseases (CVD). One of the key factors in this ongoing battle is the management of low-density lipoprotein cholesterol (LDL-C), often referred to as “bad cholesterol.” Elevated levels of LDL-C are strongly associated with an increased risk of atherosclerotic cardiovascular disease (ASCVD). The new LDL guidelines for 2024 represent a significant update, aimed at more effectively managing LDL-C levels to reduce cardiovascular risk.
Background And Importance of LDL-C
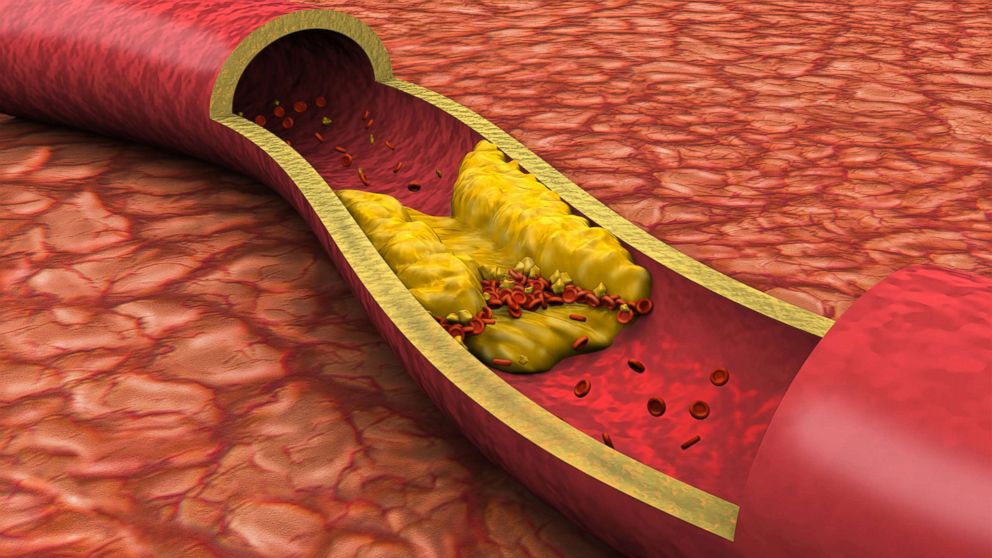
LDL-C plays a critical role in the development of atherosclerosis, a condition characterized by the buildup of cholesterol and other substances in the walls of arteries, leading to blockages that can result in heart attacks, strokes, and other serious cardiovascular conditions. Therefore, managing LDL-C levels is crucial in the prevention and treatment of ASCVD.
Key Changes in The 2024 Guidelines
The 2024 LDL guidelines introduced by the American College of Cardiology (ACC) and the American Heart Association (AHA) bring several notable updates:
SEE ALSO: What Are The Treatments for E78 Type 5 Hyperlipidemia?
Lower LDL-C Targets:
The new guidelines recommend even lower LDL-C targets for individuals at high risk of cardiovascular events. For patients with established ASCVD, the target LDL-C level is now below 55 mg/dL, compared to the previous target of below 70 mg/dL.
Stratification of Risk:
The guidelines emphasize more precise stratification of patients based on their risk of cardiovascular events. This includes using advanced risk calculators that take into account additional factors such as family history, ethnicity, and specific biomarkers.
Expanded Use of PCSK9 Inhibitors:
The guidelines endorse broader use of PCSK9 inhibitors, a class of medications that significantly lower LDL-C levels. These inhibitors are now recommended not only for patients with familial hypercholesterolemia and those who cannot achieve target LDL-C levels with statins but also for those with very high-risk ASCVD.
Non-Statin Therapies:
There is a greater emphasis on the use of non-statin therapies, such as ezetimibe and bempedoic acid, particularly in patients who are statin-intolerant or do not achieve sufficient LDL-C reduction with statins alone.
Lifestyle and Dietary Recommendations:
The guidelines continue to stress the importance of lifestyle modifications, including a heart-healthy diet, regular physical activity, weight management, and smoking cessation. These lifestyle changes are foundational for managing LDL-C levels and overall cardiovascular health.
Detailed Breakdown of The New Guidelines
Lower LDL-C Targets
One of the most significant changes in the 2024 guidelines is the adjustment of LDL-C target levels for high-risk patients.
For individuals with established ASCVD, the new target is below 55 mg/dL. This change is based on evidence from recent clinical trials that demonstrate greater cardiovascular benefits with lower LDL-C levels.
For patients with extremely high risk, such as those with multiple cardiovascular events or significant risk factors, the target may be as low as 40 mg/dL.
Risk Stratification
The guidelines now incorporate more sophisticated risk assessment tools that go beyond traditional factors like age, sex, and cholesterol levels. New models include genetic factors, specific biomarkers (such as high-sensitivity C-reactive protein and lipoprotein(a)), and socioeconomic factors. This nuanced approach allows for more personalized treatment plans and better identification of patients who may benefit from aggressive LDL-C lowering therapies.
Expanded Use of PCSK9 Inhibitors
PCSK9 inhibitors have been a game-changer in lipid management.
These injectable medications can lower LDL-C levels by 50-60%, offering an effective option for patients who are unable to reach their target levels with statins and ezetimibe alone. The 2024 guidelines recommend considering PCSK9 inhibitors earlier in the treatment process for high-risk patients, which reflects their proven efficacy and safety profile.
Non-Statin Therapies
While statins remain the cornerstone of LDL-C management, non-statin therapies are increasingly recognized for their role in comprehensive lipid-lowering strategies. Ezetimibe, which reduces cholesterol absorption in the intestine, is recommended as an add-on therapy for patients who do not achieve target LDL-C levels with statins.
Bempedoic acid, a newer oral medication that inhibits cholesterol synthesis in the liver, is also highlighted for its LDL-C lowering effects, particularly in statin-intolerant patients.
Lifestyle And Dietary Recommendations
The new guidelines reaffirm the importance of lifestyle interventions in managing LDL-C levels. Key recommendations include:
Diet: Adopting a Mediterranean-style diet, rich in fruits, vegetables, whole grains, and healthy fats, is strongly encouraged. Reducing intake of saturated fats and trans fats is essential.
Physical Activity: Engaging in at least 150 minutes of moderate-intensity aerobic exercise or 75 minutes of vigorous-intensity exercise per week is recommended.
Weight Management: Achieving and maintaining a healthy weight is crucial for reducing LDL-C levels and overall cardiovascular risk.
Smoking Cessation: Avoiding tobacco use is critical for cardiovascular health. The guidelines provide resources and support for smoking cessation programs.
Implementation And Clinical Practice
The successful implementation of these new guidelines requires a multifaceted approach. Healthcare providers must stay informed about the latest evidence and treatment options to effectively manage LDL-C levels in their patients. Shared decision-making between clinicians and patients is emphasized, ensuring that treatment plans are tailored to individual risk profiles and preferences.
Conclusion
The new LDL guidelines for 2024 represent a significant advancement in the management of cardiovascular risk. With lower LDL-C targets, improved risk stratification, expanded use of innovative therapies, and a continued emphasis on lifestyle modifications, these guidelines aim to reduce the burden of ASCVD and improve patient outcomes. As research continues to evolve, ongoing updates to guidelines will be essential to incorporate the latest evidence and optimize cardiovascular care.