Lung problems and low blood pressure, medically known as hypotension, are conditions that can significantly impact an individual’s health and quality of life. While these two health issues are commonly discussed independently, there is an intricate relationship between them that is not often explored in depth. This article aims to examine whether lung problems can cause low blood pressure, delving into the physiological connections, potential causes, and implications for treatment and management.
The Physiology of Blood Pressure And Lung Function
To understand the connection between lung problems and low blood pressure, it is essential first to grasp the basic physiology of both systems. Blood pressure is the force exerted by circulating blood on the walls of blood vessels, primarily arteries. It is regulated by various factors, including heart function, blood volume, and vascular resistance. Normal blood pressure is crucial for ensuring that all body tissues receive adequate oxygen and nutrients.
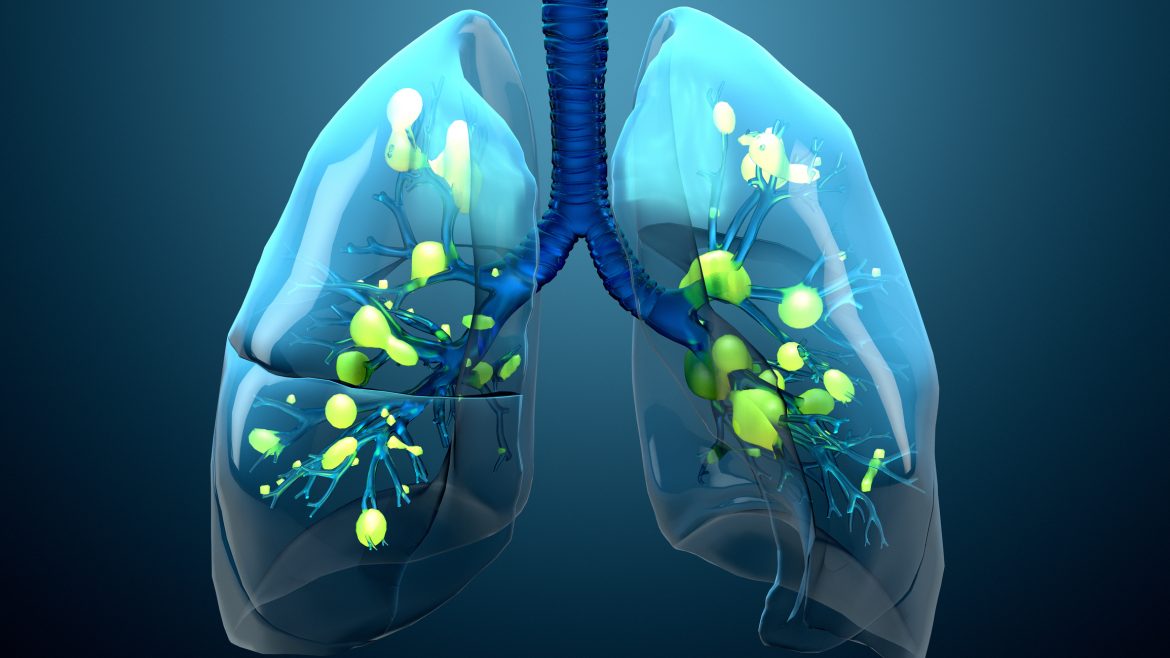
Lung function, on the other hand, involves the exchange of oxygen and carbon dioxide between the blood and the environment. This process is vital for maintaining the oxygenation of blood and the removal of carbon dioxide, a metabolic waste product. Any impairment in lung function can lead to a decrease in blood oxygen levels (hypoxemia) and an increase in carbon dioxide levels (hypercapnia), which can, in turn, affect cardiovascular function.
SEE ALSO: Why Does Heat Stroke Cause Low Blood Pressure?
Types of Lung Problems That Can Influence Blood Pressure
Several lung conditions can potentially lead to low blood pressure.
These include:
Chronic Obstructive Pulmonary Disease (COPD): COPD, which encompasses chronic bronchitis and emphysema, is characterized by obstructed airflow and impaired gas exchange. Severe COPD can lead to hypoxemia, which may result in systemic vasodilation (widening of blood vessels) and reduced blood pressure.
Pulmonary Embolism: A pulmonary embolism (PE) occurs when a blood clot blocks a pulmonary artery. This can lead to acute right ventricular failure and a drop in systemic blood pressure due to reduced cardiac output.
Pneumonia: Severe pneumonia can cause hypoxemia and systemic inflammatory responses, potentially leading to sepsis, a condition associated with low blood pressure.
Pulmonary Hypertension: While typically associated with high blood pressure in the lungs, pulmonary hypertension can lead to right heart failure, which may cause systemic hypotension in advanced stages.
Interstitial Lung Diseases: Conditions such as pulmonary fibrosis can impair gas exchange, leading to hypoxemia and potential secondary effects on blood pressure regulation.
Mechanisms Linking Lung Problems to Low Blood Pressure
Several mechanisms can explain how lung problems may lead to low blood pressure:
Hypoxemia and Vasodilation: Hypoxemia, a common feature in many lung diseases, can cause systemic vasodilation as the body attempts to improve oxygen delivery to tissues. Vasodilation decreases vascular resistance, which can lead to a drop in blood pressure.
Cardiac Output Reduction: Lung diseases can impair the right side of the heart, reducing cardiac output. For example, pulmonary embolism and pulmonary hypertension increase the workload on the right ventricle, potentially leading to heart failure and reduced blood pressure.
Systemic Inflammatory Response: Severe infections like pneumonia can trigger a systemic inflammatory response, leading to sepsis. Sepsis is characterized by widespread vasodilation, capillary leakage, and reduced effective blood volume, all of which contribute to hypotension.
Autonomic Nervous System Dysregulation: Chronic lung diseases can affect the autonomic nervous system, which regulates blood pressure. Dysregulation of this system can lead to impaired vascular tone and blood pressure control.
Clinical Implications And Management
Understanding the link between lung problems and low blood pressure has important clinical implications. Proper diagnosis and management require a comprehensive approach that addresses both the lung condition and its cardiovascular consequences.
Diagnosis
Diagnosing the cause of low blood pressure in patients with lung problems involves a thorough medical history, physical examination, and diagnostic testing. Key steps include:
Medical History and Physical Examination: A detailed history of symptoms, such as shortness of breath, chest pain, or chronic cough, can provide clues to the underlying lung condition. Physical examination findings like cyanosis (bluish discoloration of the skin), wheezing, or crackles can further guide the diagnosis.
Blood Tests: Blood tests, including arterial blood gases, can assess oxygen and carbon dioxide levels, providing insight into the severity of lung dysfunction.
Imaging Studies: Chest X-rays, CT scans, and echocardiography can help identify structural abnormalities in the lungs and heart that may contribute to low blood pressure.
Pulmonary Function Tests: These tests measure lung volumes, capacities, and gas exchange, helping to diagnose conditions like COPD and interstitial lung disease.
Treatment and Management
Effective management of low blood pressure secondary to lung problems involves addressing both the underlying lung disease and the hypotension itself. Treatment strategies may include:
Oxygen Therapy: Supplemental oxygen can improve hypoxemia, reducing the need for systemic vasodilation and potentially stabilizing blood pressure.
Medications: Depending on the underlying lung condition, medications such as bronchodilators, corticosteroids, anticoagulants, or antibiotics may be necessary. Vasopressors may be required to manage severe hypotension, particularly in cases of septic shock.
Fluid Management: Intravenous fluids can help maintain blood volume and pressure, especially in conditions like sepsis where capillary leakage is a concern.
Mechanical Ventilation: In severe cases of respiratory failure, mechanical ventilation may be necessary to ensure adequate oxygenation and support cardiac function.
Lifestyle Modifications: For chronic lung conditions, lifestyle changes such as smoking cessation, pulmonary rehabilitation, and dietary modifications can improve overall health and potentially stabilize blood pressure.
Monitoring and Follow-Up
Regular monitoring and follow-up are crucial for patients with lung problems and low blood pressure. This includes:
Frequent Blood Pressure Checks: Regular monitoring of blood pressure to detect and manage hypotension promptly.
Ongoing Assessment of Lung Function: Periodic pulmonary function tests and imaging studies to track the progression of lung disease.
Cardiovascular Monitoring: Echocardiograms and other cardiac evaluations to monitor heart function and detect any signs of right heart failure or other complications.
Patient Education: Educating patients about the signs and symptoms of worsening lung function or low blood pressure and when to seek medical attention.
Conclusion
The relationship between lung problems and low blood pressure is complex and multifaceted. Understanding the mechanisms linking these conditions is essential for accurate diagnosis and effective management. By addressing both the underlying lung disease and its cardiovascular consequences, healthcare providers can improve outcomes and quality of life for affected patients.