Coronary artery disease (CAD) remains a leading cause of morbidity and mortality worldwide, posing significant public health challenges. Understanding the factors that predispose individuals to CAD is crucial for preventive strategies, early detection, and targeted interventions. As a cardiologist specializing in arrhythmias, exploring the diverse risk factors associated with CAD provides insights into its multifactorial nature and underscores the importance of comprehensive cardiovascular risk assessment.
Epidemiology of Coronary Artery Disease
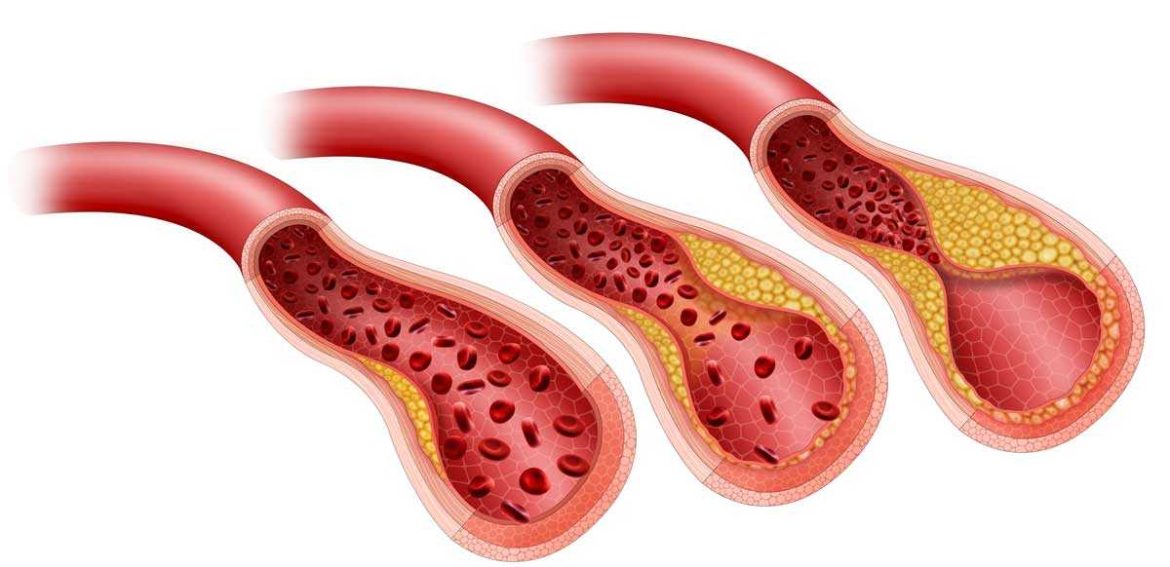
CAD encompasses a spectrum of conditions involving atherosclerosis of the coronary arteries, leading to reduced blood flow and myocardial ischemia. The prevalence of CAD varies globally but is influenced by lifestyle factors, socioeconomic status, and genetic predisposition. In developed countries, CAD is a leading cause of death, accounting for a substantial proportion of cardiovascular-related mortality.
Risk Factors for Coronary Artery Disease
Risk factors for CAD can be broadly categorized into modifiable and non-modifiable factors. Identifying these risk factors helps stratify individuals into different risk groups and guides preventive measures and therapeutic interventions.
SEE ALSO: What Are The Non-Modifiable Risk Factors for CAD?
Non-Modifiable Risk Factors
Age: Increasing age is strongly associated with a higher risk of CAD. Men aged 45 and older and women aged 55 and older are at increased risk compared to younger individuals.
Gender: Men generally have a higher risk of CAD compared to premenopausal women. However, after menopause, women’s risk increases and may approach that of men due to changes in hormonal profiles.
Family History: A family history of premature CAD (before age 55 in male relatives and before age 65 in female relatives) increases the risk of developing CAD. Genetic predisposition and shared environmental factors contribute to familial clustering of the disease.
Modifiable Risk Factors
Hypertension: High blood pressure increases the workload on the heart and accelerates atherosclerosis, leading to CAD.
Controlling blood pressure through lifestyle modifications and medications reduces cardiovascular risk.
Hyperlipidemia: Elevated levels of LDL cholesterol (“bad” cholesterol) and triglycerides, and low levels of HDL cholesterol (“good” cholesterol) contribute to atherosclerosis and CAD. Lipid-lowering therapies, including statins, are effective in reducing cardiovascular events.
Diabetes Mellitus: Diabetes significantly increases the risk of CAD due to metabolic abnormalities, including insulin resistance, dyslipidemia, and endothelial dysfunction. Tight glycemic control and cardiovascular risk factor management are essential in diabetic patients.
Smoking: Cigarette smoking is a major risk factor for CAD, accelerating atherosclerosis and increasing the risk of myocardial infarction (heart attack). Smoking cessation reduces cardiovascular risk substantially.
Obesity and Physical Inactivity: Excess body weight, particularly central obesity, and a sedentary lifestyle contribute to insulin resistance, dyslipidemia, hypertension, and inflammation, all promoting CAD. Regular physical activity and weight management are essential for cardiovascular health.
Dietary Factors: A diet high in saturated fats, trans fats, and refined carbohydrates increases the risk of CAD. Conversely, a diet rich in fruits, vegetables, whole grains, and lean proteins (Mediterranean diet) reduces cardiovascular risk.
Psychosocial Factors: Chronic stress, depression, and social isolation have been associated with an increased risk of CAD through mechanisms involving neuroendocrine pathways and unhealthy coping behaviors.
Emerging Risk Factors
In addition to traditional risk factors, several emerging factors warrant consideration in assessing CAD risk:
Inflammatory Markers: Elevated levels of inflammatory markers such as C-reactive protein (CRP) and interleukin-6 (IL-6) predict cardiovascular events and may indicate underlying vascular inflammation.
Lipoprotein(a) [Lp(a)]: Elevated Lp(a) levels are genetically determined and independently associated with increased CAD risk, particularly in individuals with premature cardiovascular disease.
Sleep Apnea: Obstructive sleep apnea is linked to hypertension, insulin resistance, and endothelial dysfunction, contributing to CAD risk.
Treatment with continuous positive airway pressure (CPAP) may mitigate cardiovascular risk.
Periodontal Disease: Poor oral health and periodontitis have been associated with increased systemic inflammation and a higher risk of CAD.
Air Pollution: Long-term exposure to air pollutants, including particulate matter (PM2.5), is associated with increased cardiovascular morbidity and mortality, possibly through oxidative stress and inflammation.
Special Populations at Risk
Certain populations face unique challenges and higher risk profiles for CAD:
Ethnic Minorities: African Americans, Hispanic Americans, South Asians, and Native Americans often experience higher rates of hypertension, diabetes, and obesity, contributing to increased CAD risk.
Women: CAD is underdiagnosed and undertreated in women compared to men, leading to poorer outcomes. Women may present with atypical symptoms or delays in seeking medical attention.
Patients with Chronic Kidney Disease (CKD): CKD is a significant risk factor for CAD due to shared pathophysiological mechanisms, including inflammation, mineral metabolism disorders, and accelerated atherosclerosis.
Cancer Survivors: Certain cancer treatments (e.g., chemotherapy, radiation therapy) may increase the risk of cardiovascular complications, including CAD, emphasizing the need for cardiovascular surveillance in cancer survivors.
Clinical Evaluation And Risk Assessment
Assessing CAD risk involves a comprehensive evaluation of traditional and emerging risk factors, clinical history, physical examination, and diagnostic testing:
Risk Assessment Tools: Calculators such as the Framingham Risk Score, ACC/AHA ASCVD Risk Estimator Plus, and the Reynolds Risk Score incorporate multiple risk factors to estimate 10-year cardiovascular risk.
Diagnostic Testing: Non-invasive tests such as coronary artery calcium scoring (CAC), stress testing (exercise or pharmacological), and coronary CT angiography (CCTA) help detect coronary artery disease and guide management decisions.
Biomarkers: Measurement of lipid profiles, inflammatory markers (e.g., hs-CRP), and novel biomarkers (e.g., Lp(a)) aids in risk stratification and personalized treatment strategies.
Prevention And Management Strategies
Preventing CAD involves targeting modifiable risk factors through lifestyle modifications and pharmacological therapies:
Lifestyle Modifications: Promoting a heart-healthy diet, regular physical activity, smoking cessation, weight management, and stress reduction.
Pharmacotherapy: Statins, anti-hypertensive medications, antiplatelet therapy (as indicated), and diabetes management to optimize cardiovascular risk reduction.
Multidisciplinary Approach: Collaborative care involving primary care providers, cardiologists, dietitians, and exercise physiologists enhances adherence to treatment goals and improves patient outcomes.
Conclusion
In conclusion, identifying individuals at risk for coronary artery disease involves a comprehensive assessment of traditional and emerging risk factors, clinical evaluation, and risk stratification tools. Modifiable risk factors such as hypertension, hyperlipidemia, diabetes, smoking, and obesity play a central role in the pathogenesis of CAD and are key targets for preventive strategies. By implementing personalized approaches to risk reduction and early intervention, healthcare providers can mitigate the burden of coronary artery disease and improve cardiovascular outcomes across diverse patient populations.