Coronary artery spasm (CAS) is a transient, sudden narrowing of the coronary arteries that can lead to chest pain, myocardial infarction, and arrhythmias. Managing and preventing these spasms is crucial for patients with this condition.
This article explores five effective ways to stop coronary artery spasm and improve cardiovascular health.
Understanding Coronary Artery Spasm
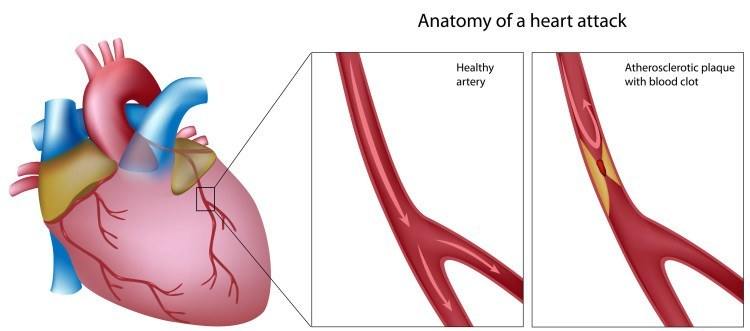
Coronary artery spasm (CAS) occurs when the muscular walls of the coronary arteries tighten and narrow, reducing blood flow to the heart muscle. This can cause angina (chest pain) and, in severe cases, myocardial infarction (heart attack). CAS can be triggered by a variety of factors, including stress, smoking, cold exposure, and certain medications. It is essential to identify and manage these triggers to prevent spasms and protect heart health.
SEE ALSO: How Long Can You Live with Congenital Heart Failure
1. Medication Management
1.1 Calcium Channel Blockers
Calcium channel blockers (CCBs) are often the first line of defense in managing CAS. These medications work by inhibiting the influx of calcium ions into the smooth muscle cells of the coronary arteries, preventing contraction and promoting dilation. Commonly prescribed CCBs include:
Amlodipine: A long-acting CCB that helps maintain consistent blood vessel relaxation.
Diltiazem: Effective in reducing the frequency and severity of spasms.
Nifedipine: Known for its potent vasodilatory effects.
1.2 Nitrates
Nitrates are another class of medications used to manage CAS. They work by relaxing the smooth muscles of the blood vessels, thus increasing blood flow to the heart. Nitrates can be used both for acute relief and long-term prevention of spasms. Common forms include:
Nitroglycerin: Often used sublingually for immediate relief during an acute spasm.
Isosorbide Mononitrate: Used for long-term management to prevent spasms.
1.3 Beta-Blockers
While beta-blockers are typically used for other types of heart conditions, their role in managing CAS is more limited due to the risk of exacerbating spasm in some patients. However, they can be beneficial in cases where CAS coexists with other cardiovascular conditions like hypertension or arrhythmias.
2. Lifestyle Modifications
2.1 Smoking Cessation
Smoking is a significant risk factor for CAS. The nicotine and other chemicals in cigarettes can induce spasm by stimulating the sympathetic nervous system and causing direct irritation to the coronary arteries. Quitting smoking is crucial for reducing the frequency and severity of spasms.
2.2 Stress Management
Stress is a common trigger for CAS. Stress management techniques can help reduce the incidence of spasms. Effective strategies include:
Mindfulness and Meditation: Practices that promote relaxation and reduce stress.
Regular Exercise: Physical activity helps manage stress and improve cardiovascular health.
Adequate Sleep: Ensuring sufficient rest can mitigate stress levels.
2.3 Diet and Nutrition
A heart-healthy diet can play a significant role in managing CAS. Key dietary recommendations include:
Reducing Sodium Intake: High sodium levels can increase blood pressure and contribute to spasms.
Increasing Omega-3 Fatty Acids: Found in fish and flaxseeds, omega-3s can help reduce inflammation and improve heart health.
Eating Plenty of Fruits and Vegetables: These provide essential vitamins, minerals, and antioxidants that support cardiovascular health.
3. Avoiding Triggers
Identifying and avoiding specific triggers is essential in managing CAS.
Common triggers include:
3.1 Cold Exposure
Cold weather can induce CAS by causing vasoconstriction. Patients should take precautions to stay warm in cold environments, such as wearing appropriate clothing and avoiding sudden temperature changes.
3.2 Certain Medications
Some medications can trigger CAS. These include:
Decongestants: Often found in over-the-counter cold medications.
Ergotamines: Used to treat migraines.
Certain Anesthetics: Used during surgical procedures.
Patients should inform their healthcare providers about their condition to avoid these medications when possible.
3.3 Excessive Alcohol Consumption
Excessive alcohol intake can provoke CAS by causing fluctuations in blood pressure and heart rate. Limiting alcohol consumption is advisable for individuals prone to spasms.
4. Regular Monitoring And Medical Follow-Up
4.1 Regular Cardiac Check-Ups
Regular visits to a cardiologist are essential for managing CAS. These check-ups allow for:
Monitoring Heart Health: Ensuring that the heart and blood vessels are functioning properly.
Adjusting Medications: Based on the patient’s response and any side effects.
Performing Diagnostic Tests: Such as ECGs, stress tests, and angiograms to assess coronary artery function.
4.2 Self-Monitoring
Patients can also play an active role in managing their condition through self-monitoring. This includes:
Keeping a Symptom Diary: Recording instances of chest pain, triggers, and relief measures.
Monitoring Blood Pressure: Keeping track of blood pressure at home to detect any changes that might indicate a spasm.
Using Personal Health Devices: Wearable devices can help monitor heart rate and other vital signs.
5. Advanced Therapeutic Options
5.1 Enhanced External Counterpulsation (EECP)
EECP is a non-invasive treatment that can help improve blood flow to the heart. It involves the use of inflatable cuffs placed around the legs that compress and decompress in sync with the heartbeat, promoting increased blood flow through the coronary arteries. EECP has been shown to reduce angina episodes and improve exercise tolerance in patients with CAS.
5.2 Coronary Stenting
In cases where CAS is associated with significant coronary artery disease, coronary stenting may be necessary. A stent is a small mesh tube inserted into the coronary artery to keep it open and ensure adequate blood flow. This procedure can provide long-term relief from spasms and prevent future episodes.
5.3 Lifestyle Intervention Programs
Comprehensive lifestyle intervention programs that combine diet, exercise, stress management, and education can significantly improve outcomes for patients with CAS. These programs provide a structured approach to making and sustaining lifestyle changes that promote heart health.
5.4 Alternative Therapies
Some patients may find relief through alternative therapies such as:
Acupuncture: Can help reduce stress and improve circulation.
Herbal Supplements: Certain herbs like hawthorn and ginkgo biloba have been suggested to support cardiovascular health, though patients should consult their healthcare provider before starting any supplements.
Conclusion
Coronary artery spasm is a challenging condition that requires a multifaceted approach to management. By combining medication, lifestyle modifications, trigger avoidance, regular monitoring, and advanced therapeutic options, patients can effectively manage their condition and improve their quality of life. It is essential for individuals with CAS to work closely with their healthcare providers to develop a personalized treatment plan that addresses their unique needs and circumstances.