Myocarditis is an inflammatory condition of the myocardium, the heart muscle, often resulting from infections, immune-mediated mechanisms, or toxic substances. The clinical presentation of myocarditis can be highly variable, ranging from asymptomatic to severe heart failure and sudden cardiac death. This variability, coupled with its non-specific symptoms and the limitations of current diagnostic tools, can make myocarditis challenging to diagnose accurately. As a result, several other conditions may be easily misdiagnosed as myocarditis. This article explores the conditions that are commonly mistaken for myocarditis and the reasons behind these diagnostic challenges.
What Conditions Are Easily Misdiagnosed as Myocarditis?
1. Acute Coronary Syndrome (ACS)
Similarities:
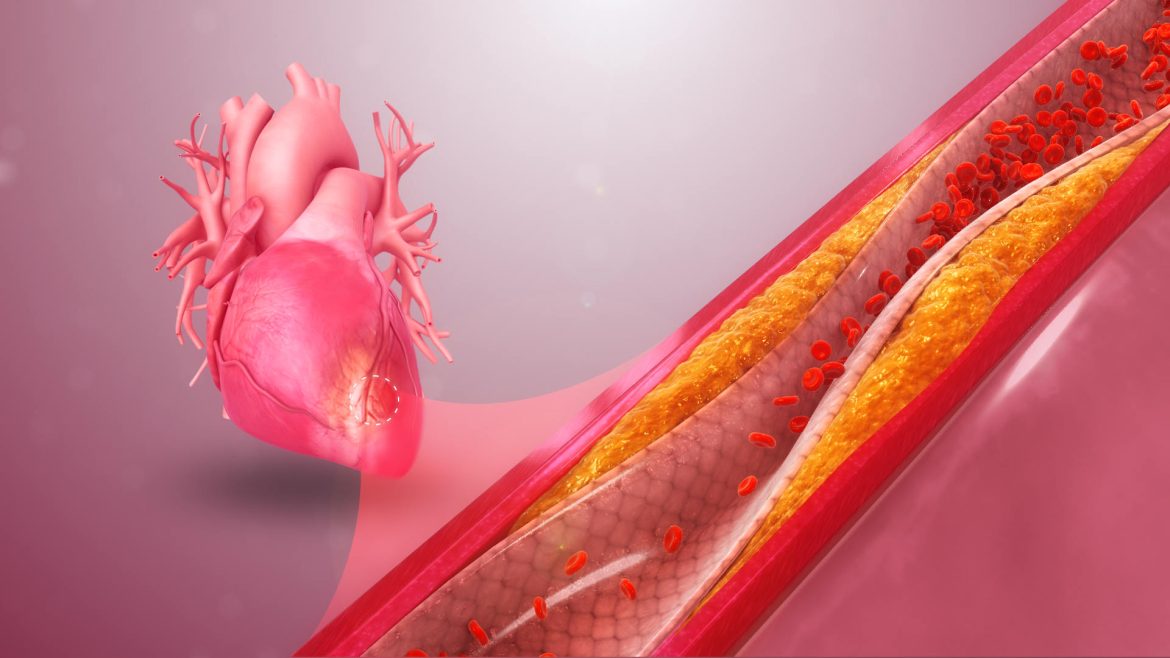
Acute coronary syndrome (ACS) encompasses a range of conditions associated with sudden, reduced blood flow to the heart, including myocardial infarction (heart attack) and unstable angina. Both myocarditis and ACS can present with chest pain, elevated cardiac biomarkers (such as troponins), and electrocardiographic (ECG) changes.
Differences:
While ACS is typically characterized by atherosclerotic plaque rupture and thrombus formation, myocarditis involves inflammation of the heart muscle. Coronary angiography, which visualizes the coronary arteries, can help differentiate ACS from myocarditis. In ACS, angiography often reveals significant coronary artery disease, whereas, in myocarditis, the coronary arteries usually appear normal.
SEE ALSO: Does The J&J Vaccine Cause Myocarditis?
2. Pericarditis
Similarities:
Pericarditis, an inflammation of the pericardium (the sac surrounding the heart), can present with chest pain, ECG changes (such as ST-segment elevation), and elevated inflammatory markers. These symptoms can overlap significantly with those of myocarditis.
Differences:
The key distinguishing feature of pericarditis is the presence of a pericardial friction rub, a characteristic sound heard on auscultation.
Additionally, imaging studies such as echocardiography can reveal pericardial effusion (fluid around the heart), which is more common in pericarditis than in myocarditis. MRI can also help differentiate between the two by identifying inflammation in the myocardium versus the pericardium.
3. Dilated Cardiomyopathy (DCM)
Similarities:
Dilated cardiomyopathy (DCM) is a condition where the heart becomes enlarged and weakened, leading to impaired pumping ability.
Myocarditis can sometimes progress to a dilated cardiomyopathy phenotype, making differentiation challenging. Both conditions can present with heart failure symptoms, such as shortness of breath, fatigue, and edema.
Differences:
The etiology of DCM is often idiopathic, genetic, or related to other systemic diseases, whereas myocarditis typically has an identifiable inflammatory cause. Endomyocardial biopsy and cardiac MRI can provide critical information to distinguish DCM from active myocarditis by identifying ongoing inflammation in myocarditis.
4. Sarcoidosis
Similarities:
Cardiac sarcoidosis, an inflammatory disease that leads to granuloma formation in the heart, can mimic myocarditis both clinically and on imaging studies. Patients may present with heart failure, arrhythmias, or conduction disturbances.
Differences:
The presence of non-caseating granulomas on biopsy is a hallmark of sarcoidosis. Advanced imaging techniques, such as cardiac MRI and PET scans, can help identify characteristic patterns of sarcoidosis, such as late gadolinium enhancement in a patchy distribution.
Systemic involvement of sarcoidosis in other organs, such as the lungs, can also aid in the diagnosis.
5. Stress Cardiomyopathy (Takotsubo Syndrome)
Similarities:
Stress cardiomyopathy, also known as Takotsubo syndrome, is characterized by transient left ventricular dysfunction often triggered by emotional or physical stress. It can present with chest pain, ECG changes, and elevated cardiac biomarkers, similar to myocarditis.
Differences:
Takotsubo syndrome typically shows a distinctive apical ballooning pattern on echocardiography or ventriculography, where the apex of the heart bulges out while the base contracts normally. This pattern helps differentiate it from myocarditis. Additionally, coronary angiography usually shows no significant coronary artery disease in Takotsubo syndrome.
6. Hypertrophic Cardiomyopathy (HCM)
Similarities:
Hypertrophic cardiomyopathy (HCM) is a genetic condition characterized by thickened heart muscle. It can present with symptoms such as chest pain, palpitations, and shortness of breath, which overlap with those of myocarditis.
Differences:
Echocardiography is crucial in differentiating HCM from myocarditis by identifying asymmetric septal hypertrophy, which is characteristic of HCM. Genetic testing and family history can also provide important clues, as HCM is often hereditary.
7. Infective Endocarditis
Similarities:
Infective endocarditis, an infection of the heart valves, can present with fever, heart murmur, and embolic phenomena, which can be confused with myocarditis, especially if the infection spreads to the myocardium.
Differences:
Blood cultures and echocardiography are essential in diagnosing infective endocarditis, revealing vegetations on the heart valves. The presence of positive blood cultures and valve involvement helps distinguish infective endocarditis from myocarditis.
8. Autoimmune Diseases
Similarities:
Autoimmune diseases such as systemic lupus erythematosus (SLE) and rheumatoid arthritis (RA) can involve the heart, leading to symptoms similar to myocarditis, including chest pain and heart failure.
Differences:
The presence of systemic manifestations, such as joint involvement, skin rashes, and specific autoantibodies, can help differentiate autoimmune diseases from myocarditis. Cardiac involvement in autoimmune diseases often shows a different pattern on imaging and biopsy compared to myocarditis.
Diagnostic Tools And Approaches
Accurate diagnosis of myocarditis requires a combination of clinical evaluation, imaging, laboratory tests, and sometimes endomyocardial biopsy. The following diagnostic tools are commonly used:
1. Electrocardiogram (ECG)
ECG can reveal nonspecific changes such as ST-segment elevation, T-wave inversions, or arrhythmias. While these findings are not specific to myocarditis, they provide important initial clues.
2. Cardiac Biomarkers
Elevated levels of cardiac troponins and other biomarkers indicate myocardial injury but do not differentiate between myocarditis and other causes of myocardial damage.
3. Echocardiography
Echocardiography is useful for assessing cardiac function and detecting pericardial effusion or ventricular dysfunction.
However, it may not provide definitive evidence of myocarditis.
4. Cardiac MRI
Cardiac MRI is a valuable tool for diagnosing myocarditis, as it can detect myocardial edema, hyperemia, and fibrosis. Late gadolinium enhancement on MRI is particularly useful in identifying areas of inflammation and scarring.
5. Endomyocardial Biopsy
Endomyocardial biopsy is the gold standard for diagnosing myocarditis, as it allows direct examination of myocardial tissue.
However, it is an invasive procedure and may not always be feasible or necessary.
6. Laboratory Tests
Blood tests, including inflammatory markers (CRP, ESR) and viral serologies, can provide supportive evidence for myocarditis.
Autoantibody tests can help identify autoimmune causes.
7. Advanced Imaging
In cases of suspected sarcoidosis or other systemic diseases, advanced imaging techniques such as PET scans may be used to detect extracardiac involvement.
Conclusion
Diagnosing myocarditis can be challenging due to its nonspecific symptoms and the overlap with various other cardiac and systemic conditions. Acute coronary syndrome, pericarditis, dilated cardiomyopathy, sarcoidosis, stress cardiomyopathy, hypertrophic cardiomyopathy, infective endocarditis, and autoimmune diseases are some of the conditions that can be easily misdiagnosed as myocarditis. A thorough clinical evaluation, combined with advanced imaging, laboratory tests, and sometimes biopsy, is essential for accurate diagnosis.