Cardiac spasms, also known as coronary artery spasms or Prinzmetal’s angina, are sudden, temporary tightening or constriction of the muscles within the walls of the arteries that supply blood to the heart. This phenomenon can reduce or completely block blood flow to part of the heart muscle, leading to chest pain, arrhythmias, or even heart attacks.
Understanding the causes of cardiac spasms is crucial for effective prevention and management. This article explores the various factors that can trigger cardiac spasms, including lifestyle choices, medical conditions, and environmental influences.
Pathophysiology of Cardiac Spasms
To grasp what causes cardiac spasms, it’s essential to understand the underlying pathophysiology. The heart’s blood supply is maintained by the coronary arteries. Under normal conditions, these arteries expand and contract to regulate blood flow based on the heart’s needs.
However, in the case of a spasm, the smooth muscles in the arterial walls contract abnormally, leading to a temporary but significant reduction in blood flow.
The precise mechanisms causing these spasms are not entirely understood, but several factors and conditions have been identified as potential contributors.
SEE ALSO: 5 Ways to Stop Coronary Artery Spasm
What Causes Cardiac Spasms?
Lifestyle Factors
Smoking
Smoking is one of the most significant lifestyle factors associated with cardiac spasms. Nicotine and other chemicals in cigarettes can cause the coronary arteries to constrict, reducing blood flow to the heart.
Additionally, smoking contributes to atherosclerosis (the buildup of plaques in the arteries), which can make the arteries more prone to spasms.
Stress
Emotional stress and anxiety are well-documented triggers of cardiac spasms. Stress stimulates the release of catecholamines (such as adrenaline), which can lead to increased heart rate and blood pressure.
This hormonal surge can cause the coronary arteries to constrict, precipitating a spasm.
Alcohol Consumption
Excessive alcohol consumption is another lifestyle factor that can precipitate cardiac spasms. Alcohol can affect the smooth muscle tone of the coronary arteries and lead to their constriction. Binge drinking, in particular, is a known trigger for coronary artery spasms.
Diet
A diet high in unhealthy fats and low in essential nutrients can contribute to the development of atherosclerosis, making the coronary arteries more susceptible to spasms. Additionally, certain foods and beverages, such as caffeine, can provoke spasms in some individuals.
Medical Conditions
Atherosclerosis
Atherosclerosis is a significant underlying condition that can predispose individuals to cardiac spasms. Plaque buildup in the arteries not only narrows them but also makes them more reactive to constrictive stimuli. The presence of atherosclerosis means the arteries are less flexible and more prone to spasmodic reactions.
High blood pressure is a known risk factor for many cardiovascular conditions, including cardiac spasms. Hypertension can damage the arteries over time, making them more susceptible to spasms. The increased pressure on the arterial walls can also trigger spasmodic reactions.
Elevated levels of cholesterol and triglycerides in the blood (hyperlipidemia) contribute to the formation of atherosclerotic plaques.
These plaques can make the coronary arteries more prone to spasms, especially in response to various stimuli like cold exposure or stress.
Diabetes
Diabetes is associated with endothelial dysfunction, which can affect the smooth muscle function in the coronary arteries.
This dysfunction can lead to an increased risk of spasms. Moreover, diabetes accelerates the process of atherosclerosis, further predisposing individuals to cardiac spasms.
Autoimmune Diseases
Certain autoimmune diseases, such as lupus and rheumatoid arthritis, can increase the risk of cardiac spasms. These conditions often involve chronic inflammation, which can affect the coronary arteries’ function and increase their susceptibility to spasms.
Migraine
There is a documented link between migraines and cardiac spasms.
Both conditions may involve similar mechanisms, such as abnormal smooth muscle function and vascular reactivity. People with migraines, particularly those with aura, may be at higher risk for cardiac spasms.
Environmental Influences
Cold Exposure
Exposure to cold temperatures can trigger cardiac spasms. Cold weather causes the blood vessels to constrict in an effort to preserve body heat, which can inadvertently lead to coronary artery spasms.
This is particularly concerning for individuals with pre-existing cardiovascular conditions.
Drug Use
The use of certain drugs, both prescription and recreational, can precipitate cardiac spasms. For instance, cocaine is a well-known trigger due to its potent vasoconstrictive properties. Some medications, such as certain vasodilators used for treating migraines or erectile dysfunction, can paradoxically cause spasms in susceptible individuals.
Allergic Reactions
Severe allergic reactions (anaphylaxis) can lead to cardiac spasms.
During an allergic reaction, the body releases large amounts of histamine and other chemicals that can cause widespread vasoconstriction, including in the coronary arteries.
Genetic Factors
Genetic Predisposition
Genetics can play a role in an individual’s susceptibility to cardiac spasms. Certain genetic mutations and hereditary conditions can affect the vascular smooth muscle function and reactivity, predisposing individuals to spasmodic episodes.
Family History
A family history of cardiovascular diseases, including coronary artery spasms, can indicate a higher risk for developing similar conditions.
Genetic and lifestyle factors within families can contribute to this increased risk.
Diagnosis And Management
Diagnosis
Diagnosing cardiac spasms typically involves a combination of clinical evaluation, patient history, and diagnostic tests.
Common diagnostic methods include:
Electrocardiogram (ECG): To detect changes in the heart’s electrical activity during a spasm.
Holter Monitor: A portable ECG device worn for 24-48 hours to capture intermittent spasms.
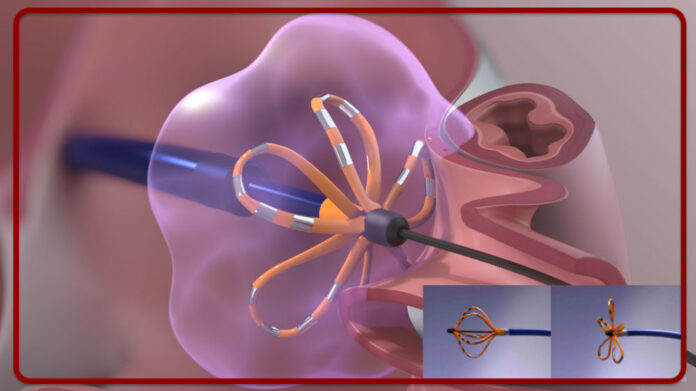
Coronary Angiography: An imaging test that uses a contrast dye to visualize the coronary arteries.
Ergonovine Provocation Test: A test where a medication is administered to provoke a spasm under controlled conditions.
Management
Managing cardiac spasms involves addressing both the acute symptoms and the underlying causes. Treatment strategies may include:
Medications: Calcium channel blockers and nitrates are commonly used to relax the coronary arteries and prevent spasms.
Lifestyle Modifications: Quitting smoking, reducing alcohol consumption, managing stress, and adopting a heart-healthy diet can significantly reduce the risk of spasms.
Avoiding Triggers: Identifying and avoiding known triggers, such as cold exposure and certain medications, can help prevent spasmodic episodes.
Conclusion
Cardiac spasms are a complex condition with multiple contributing factors, including lifestyle choices, medical conditions, environmental influences, and genetic predispositions. Understanding these triggers is crucial for effective prevention and management. By addressing the underlying causes and adopting a comprehensive approach to treatment, individuals can reduce their risk of cardiac spasms and maintain better heart health.