Heart stents are crucial devices used to treat blocked coronary arteries. These small mesh tubes help keep arteries open and ensure proper blood flow to the heart. While stents are generally effective and have significantly improved outcomes for patients with coronary artery disease, they are not without risks. Stent failure, although relatively rare, can have serious consequences. Understanding what happens when a heart stent fails is essential for patients and healthcare providers to manage and mitigate potential complications effectively.
Understanding Heart Stents
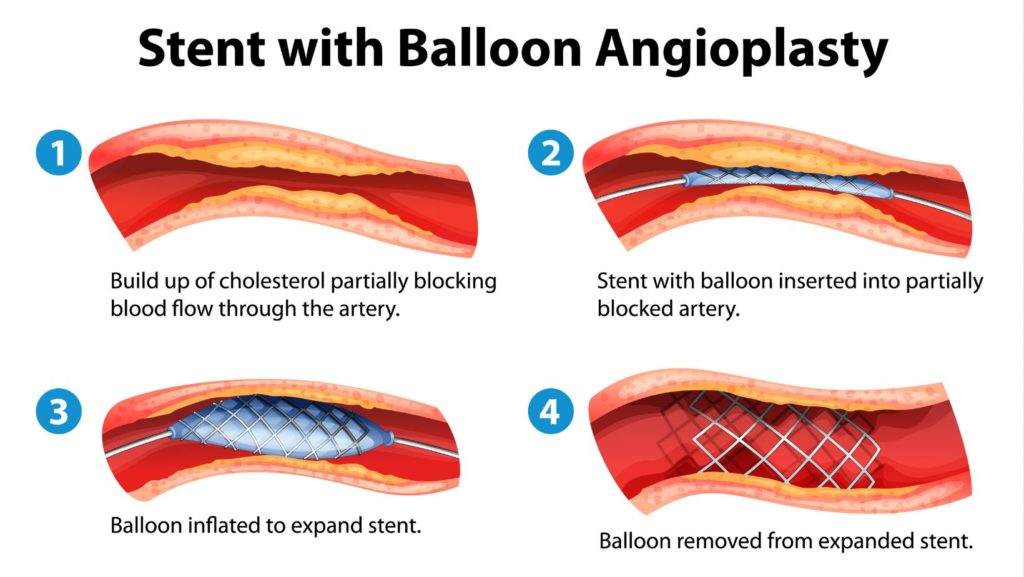
Heart stents are typically used in a procedure called percutaneous coronary intervention (PCI), also known as angioplasty.
During PCI, a balloon is used to open the blocked artery, and the stent is then placed to keep it open. There are two main types of stents: bare-metal stents (BMS) and drug-eluting stents (DES). BMS are simple metal tubes, while DES are coated with medication that helps prevent the artery from becoming blocked again.
SEE ALSO: Can Exercise Repair Heart Damage?
Types of Stent Failure
Stent failure can occur in several ways, each with its own set of implications and required interventions. The main types of stent failure include:
Stent Thrombosis: This is a rare but severe complication where a blood clot forms inside the stent, leading to a sudden blockage of the artery. Stent thrombosis can occur at any time after stent placement but is most critical in the first few months.
In-Stent Restenosis: This occurs when scar tissue grows inside the stent, leading to re-narrowing of the artery. In-stent restenosis typically develops months or years after the initial stent placement.
Stent Fracture: Although rare, stents can sometimes break or fracture, which can compromise their effectiveness and lead to artery re-blockage or other complications.
Stent Migration: This happens when the stent moves from its original position, which can cause artery damage or re-blockage.
Causes of Stent Failure
Several factors can contribute to stent failure, including:
Patient-Related Factors: Conditions such as diabetes, chronic kidney disease, and smoking can increase the risk of stent failure. Non-adherence to prescribed medications, such as antiplatelet drugs, can also contribute to complications.
Procedure-Related Factors: Inadequate stent placement, suboptimal stent expansion, or improper choice of stent size can lead to failure.
Technical issues during the procedure can also play a role.
Biological Factors: The body’s response to the stent, including inflammation and excessive scar tissue formation, can result in restenosis.
Mechanical Factors: Stent fractures or deformation due to excessive movement or pressure can lead to failure.
What Happens When A Heart Stent Fails
When a heart stent fails, it can manifest through various symptoms, including:
Chest Pain (Angina): This is the most common symptom, indicating that the heart is not receiving enough blood. The pain may resemble the original symptoms experienced before the stent placement.
Shortness of Breath: Difficulty breathing or shortness of breath can occur if the heart is not getting sufficient oxygenated blood.
Heart Attack: In severe cases, especially with stent thrombosis, a heart attack can occur, presenting with intense chest pain, sweating, nausea, and other symptoms.
Fatigue: Generalized fatigue or a feeling of being unwell can indicate reduced cardiac function.
Diagnosing Stent Failure
If stent failure is suspected, several diagnostic tests can be employed:
Electrocardiogram (ECG): This test records the electrical activity of the heart and can indicate areas of reduced blood flow or heart attack.
Stress Testing: This involves exercising or taking medication to make the heart work harder while monitoring its activity, helping to detect issues with blood flow.
Coronary Angiography: This is the most definitive test, involving the injection of contrast dye into the coronary arteries followed by X-ray imaging to visualize blockages or stent issues.
Intravascular Ultrasound (IVUS): This imaging technique uses a tiny ultrasound probe on a catheter inserted into the coronary arteries to provide detailed images of the stent and artery walls.
Treatment Options for Stent Failure
The treatment for stent failure depends on the type and severity of the failure:
Medications: For minor cases or early signs of restenosis, medications such as antiplatelet drugs, cholesterol-lowering agents, and anti-inflammatory drugs may be used to manage symptoms and prevent further complications.
Repeat Angioplasty and Stenting: In cases of significant restenosis or thrombosis, a repeat PCI procedure may be necessary.
This can involve balloon angioplasty to re-open the artery or placing an additional stent.
Brachytherapy: This is a specialized treatment for in-stent restenosis, involving the delivery of radiation directly to the affected area to inhibit scar tissue formation.
Coronary Artery Bypass Grafting (CABG): In severe cases or when repeat stenting is not viable, bypass surgery may be required to create a new pathway for blood flow around the blocked artery.
Preventing Stent Failure
Preventing stent failure involves a combination of lifestyle changes, medication adherence, and regular medical follow-up:
Lifestyle Modifications: Quitting smoking, maintaining a healthy diet, exercising regularly, and managing stress can significantly reduce the risk of stent failure and improve overall cardiovascular health.
Medication Adherence: Strictly following prescribed medication regimens, particularly antiplatelet therapy, is crucial in preventing stent thrombosis and restenosis.
Regular Check-Ups: Regular follow-up appointments with a cardiologist and routine tests can help monitor the stent’s condition and catch any issues early.
Managing Comorbidities: Proper management of conditions like diabetes, hypertension, and high cholesterol is essential to reduce the risk of complications.
Conclusion
Heart stents are life-saving devices that have revolutionized the treatment of coronary artery disease. However, stent failure, though uncommon, can have serious repercussions. Understanding the types, causes, symptoms, and treatment options for stent failure is crucial for patients and healthcare providers. Through preventive measures, regular monitoring, and timely intervention, the risks associated with stent failure can be minimized, ensuring better outcomes and improved quality of life for patients with coronary artery disease.