An electrocardiogram (EKG or ECG) is a fundamental diagnostic tool in cardiology, widely used to assess the electrical activity of the heart. It provides critical information about heart rhythm, conduction abnormalities, and myocardial ischemia. One of the key questions that often arises is whether an EKG can detect a heart blockage.
Understanding the capabilities and limitations of an EKG in diagnosing heart blockages is essential for both clinicians and patients.
What Is Heart Blockages?
Heart blockages, often referred to as coronary artery disease (CAD), occur when the coronary arteries, which supply blood to the heart muscle, become narrowed or blocked due to the buildup of plaque.
This plaque is composed of fat, cholesterol, and other substances.
Over time, the accumulation of plaque can reduce blood flow to the heart muscle, potentially leading to chest pain (angina), shortness of breath, heart attack, or other serious complications.
SEE ALSO: How Long Can You Live with Moderate Aortic Stenosis
Types of Heart Blockages
There are several types of heart blockages, which can vary in severity:
Partial Blockage (Stable Angina): When a coronary artery is partially blocked, it can cause stable angina, characterized by chest pain that occurs during exertion and is relieved by rest.
Complete Blockage (Myocardial Infarction): A complete blockage can lead to a heart attack (myocardial infarction), where a portion of the heart muscle is deprived of oxygen and begins to die.
Unstable Blockage (Unstable Angina): Unstable angina occurs when a blockage suddenly worsens, leading to chest pain at rest or with minimal exertion. This is a medical emergency and can precede a heart attack.
Silent Blockage: Some blockages do not cause noticeable symptoms and are only detected through diagnostic tests or during an evaluation for another condition.
Role of An EKG in Detecting Heart Blockages
An EKG records the electrical activity of the heart through electrodes placed on the skin. It produces a waveform that represents the depolarization and repolarization of the heart muscle. While an EKG is a powerful tool, its ability to detect heart blockages directly is limited. However, it can provide indirect evidence of blockages through several mechanisms.
Identifying Ischemia and Infarction
ST Segment Changes: One of the most significant indicators of a heart blockage on an EKG is the presence of ST segment changes. ST segment elevation can suggest an acute myocardial infarction, indicating a complete blockage of a coronary artery. Conversely, ST segment depression or T wave inversions can indicate myocardial ischemia, often due to a partial blockage.
Q Waves: Pathological Q waves on an EKG can indicate a previous myocardial infarction, suggesting that a blockage may have occurred in the past. These waves typically appear after the infarcted area has healed and can signify the location and extent of the damage.
T Wave Abnormalities: T wave inversions or flattening can be indicative of ischemia or infarction. While not specific to heart blockages, these changes warrant further investigation.
Detecting Arrhythmias
Heart blockages can lead to various arrhythmias, which an EKG can detect. For example, ischemia from a blockage can cause ventricular arrhythmias, such as ventricular tachycardia or fibrillation, which are life-threatening conditions. Additionally, atrial fibrillation can be associated with CAD.
Limitations of An EKG
While an EKG can provide valuable information about heart health, it has limitations in diagnosing heart blockages:
Normal EKG in CAD: It is possible for individuals with significant coronary artery disease to have a normal EKG at rest.
EKG changes may only occur during stress or exertion when the heart demands more oxygen.
Non-Specific Findings: Some EKG changes, such as nonspecific ST-T wave changes, can be caused by various conditions, not just heart blockages. Therefore, an EKG alone is not definitive for diagnosing CAD.
Transient Changes: Ischemic changes on an EKG can be transient and may not be present at the time of the recording.
Continuous monitoring or stress testing may be necessary to capture these changes.
Complementary Diagnostic Tools
Given the limitations of an EKG, other diagnostic tests are often used in conjunction to evaluate for heart blockages:
Stress Testing: Stress tests, including exercise stress tests and pharmacological stress tests, monitor the heart’s response to increased demand. Changes in the EKG during stress can indicate ischemia and suggest the presence of blockages.
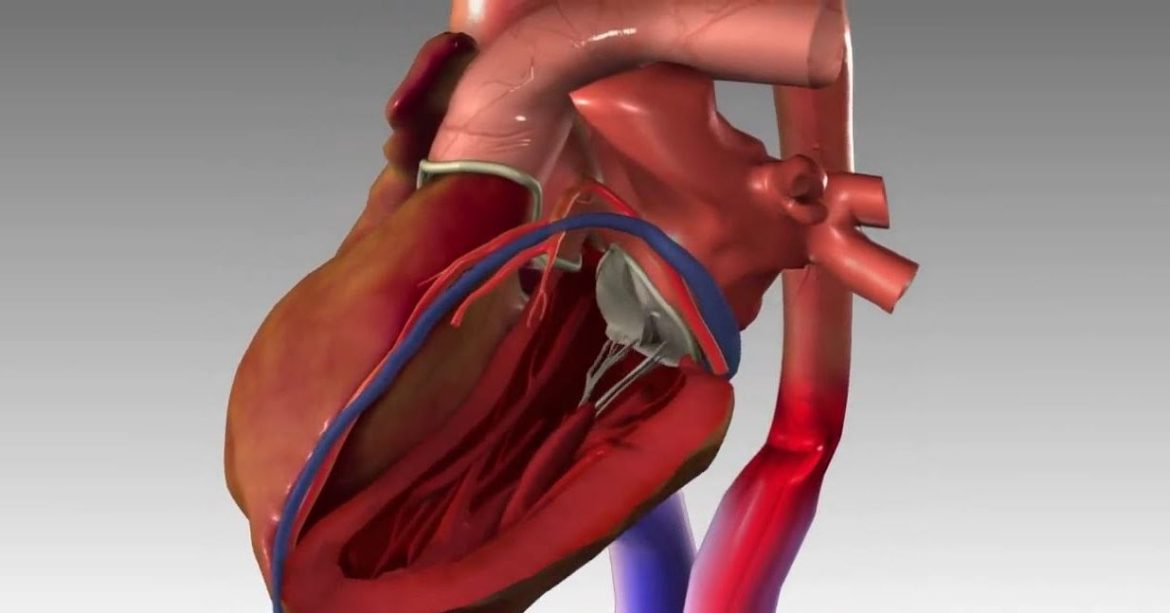
Echocardiography: This ultrasound-based test provides images of the heart’s structure and function. It can identify areas of the heart that are not receiving enough blood flow due to blockages.
Nuclear Imaging: Techniques like myocardial perfusion imaging involve injecting a radioactive tracer and capturing images of blood flow to the heart muscle. Reduced uptake in certain areas can indicate blockages.
Coronary Angiography: This invasive procedure involves injecting contrast dye into the coronary arteries and taking X-ray images. It provides a detailed view of the coronary arteries and can directly visualize blockages.
CT Coronary Angiography: A non-invasive alternative to traditional angiography, CT coronary angiography uses computed tomography to create detailed images of the coronary arteries and detect blockages.
Clinical Application And Interpretation
When interpreting an EKG in the context of suspected heart blockages, clinicians consider the patient’s symptoms, risk factors, and overall clinical picture. Here are some scenarios where an EKG is particularly useful:
Acute Coronary Syndrome (ACS)
In patients presenting with chest pain, an EKG is performed immediately to evaluate for ACS. ST segment elevation suggests an ST-elevation myocardial infarction (STEMI), warranting urgent intervention to restore blood flow. ST segment depression or T wave inversions may indicate non-ST-elevation myocardial infarction (NSTEMI) or unstable angina, which also require prompt management.
Chronic Stable Angina
For patients with chronic stable angina, an EKG may be normal at rest. However, stress testing with EKG monitoring can reveal ischemic changes during exertion, guiding further investigation and treatment.
Silent Ischemia
In some cases, patients may have silent ischemia, where they do not experience typical symptoms despite having significant blockages. An EKG may show ischemic changes, prompting further evaluation with stress testing or imaging.
Post-Myocardial Infarction
After a myocardial infarction, an EKG can help assess the extent of damage and monitor for complications such as arrhythmias.
Pathological Q waves, ST segment changes, and T wave abnormalities provide information about the infarcted area.
Conclusion
An EKG is a valuable tool in the detection and management of heart blockages, but it has its limitations. While it can provide indirect evidence of blockages through ischemic changes, arrhythmias, and infarction patterns, it is not definitive for diagnosing coronary artery disease. Complementary tests such as stress testing, echocardiography, nuclear imaging, and coronary angiography are often necessary for a comprehensive evaluation.