An arterial tear in the heart, also known as a coronary artery dissection or spontaneous coronary artery dissection (SCAD), is a serious and potentially life-threatening condition. It occurs when a tear forms in the wall of a coronary artery, leading to a range of cardiovascular complications. Understanding the causes of this condition is critical for prevention, early detection, and effective treatment. This article explores the various factors that can lead to an arterial tear in the heart, shedding light on the mechanisms behind this medical emergency.
Anatomy And Function of Coronary Arteries
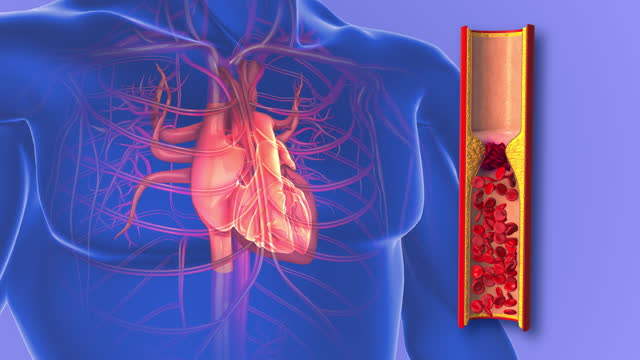
The coronary arteries are vital blood vessels that supply oxygen-rich blood to the heart muscle. They branch off from the aorta and encircle the heart, ensuring that it receives the necessary nutrients and oxygen to function effectively. The walls of the coronary arteries are composed of three layers: the intima (inner layer), the media (middle layer), and the adventitia (outer layer). A tear can occur in any of these layers, disrupting the blood flow and potentially leading to a heart attack or other severe cardiac events.
Primary Causes of Arterial Tears
Spontaneous Coronary Artery Dissection (SCAD)
SCAD is one of the primary causes of arterial tears in the heart. This condition occurs without any prior trauma or external force. SCAD is more common in women, particularly those who are young and otherwise healthy. The exact cause of SCAD is not fully understood, but several factors may contribute to its occurrence:
Hormonal Changes: Hormonal fluctuations, particularly those related to pregnancy and childbirth, can weaken the arterial walls, making them more susceptible to tearing.
Fibromuscular Dysplasia (FMD): This condition causes abnormal cell growth in the arterial walls, leading to irregularities and weakness that can result in tears.
Genetic Predisposition: Some individuals may have a genetic predisposition to SCAD, although the specific genetic factors involved are still being studied.
SEE ALSO: How Much Percentage of Heart Blockage Is Normal?
Atherosclerosis
Atherosclerosis, the buildup of plaque in the arteries, is a common cause of arterial tears. Plaque is composed of cholesterol, fatty substances, cellular waste products, calcium, and fibrin. Over time, plaque can harden and narrow the arteries, reducing blood flow. The following factors contribute to atherosclerosis:
High Cholesterol: Elevated levels of low-density lipoprotein (LDL) cholesterol can lead to plaque formation in the arteries.
Hypertension: High blood pressure can damage the arterial walls, making them more prone to plaque buildup and subsequent tears.
Smoking: Tobacco smoke contains chemicals that damage the lining of the arteries, promoting plaque formation and increasing the risk of arterial tears.
Diabetes: High blood sugar levels can damage the arteries and accelerate the process of atherosclerosis.
Trauma and Physical Injury
Direct trauma or physical injury to the chest can cause a tear in the coronary arteries. This can result from accidents, falls, or blunt force impact. The force exerted on the chest can damage the arterial walls, leading to a tear and subsequent complications.
Connective Tissue Disorders
Certain connective tissue disorders can weaken the arterial walls, making them more susceptible to tears. These disorders include:
Marfan Syndrome: A genetic disorder that affects the body’s connective tissue, leading to weakened blood vessels and an increased risk of arterial tears.
Ehlers-Danlos Syndrome: A group of genetic disorders that affect the connective tissue, causing skin hyperelasticity, joint hypermobility, and fragile blood vessels.
Inflammatory Conditions
Inflammatory conditions can also contribute to the weakening of the arterial walls, increasing the risk of tears. These conditions include:
Vasculitis: Inflammation of the blood vessels can cause damage to the arterial walls, making them more prone to tearing.
Lupus: An autoimmune disease that can cause inflammation and damage to various organs, including the arteries.
Secondary Factors Contributing to Arterial Tears
Stress and Emotional Factors
Acute emotional stress and intense physical exertion can trigger arterial tears, especially in individuals with underlying conditions such as SCAD or atherosclerosis. The sudden increase in blood pressure and heart rate during stress can put additional strain on the arterial walls, leading to a tear.
Medication and Substance Use
Certain medications and substances can weaken the arterial walls or increase the risk of a tear. These include:
Oral Contraceptives: Hormonal birth control pills can increase the risk of blood clots and arterial tears, particularly in women with other risk factors.
Cocaine and Amphetamines: These stimulants can cause severe vasoconstriction and increase blood pressure, leading to damage and tears in the arterial walls.
Pregnancy and Postpartum Period
Pregnancy and the postpartum period are times of significant hormonal and physiological changes, which can increase the risk of SCAD. The increased blood volume and hormonal fluctuations during pregnancy can weaken the arterial walls, making them more susceptible to tears.
Symptoms And Diagnosis
Recognizing the symptoms of an arterial tear in the heart is crucial for prompt medical intervention. The symptoms can vary depending on the severity and location of the tear but often include:
Chest Pain: Sudden, severe chest pain that may radiate to the back, neck, or arms.
Shortness of Breath: Difficulty breathing or a feeling of tightness in the chest.
Nausea and Vomiting: These symptoms can accompany chest pain and may be mistaken for gastrointestinal issues.
Dizziness or Fainting: A tear in the coronary artery can lead to reduced blood flow to the brain, causing dizziness or fainting.
To diagnose an arterial tear, healthcare professionals may use various imaging techniques, including:
Coronary Angiography: This procedure involves injecting a contrast dye into the coronary arteries to visualize the blood flow and identify any tears or blockages.
Computed Tomography (CT) Angiography: A non-invasive imaging technique that provides detailed images of the coronary arteries.
Magnetic Resonance Imaging (MRI): This imaging modality can help identify tears and assess the extent of damage to the arterial walls.
Treatment And Management
The treatment and management of an arterial tear in the heart depend on the severity of the condition and the underlying cause. Treatment options may include:
Medications
Antiplatelet and Anticoagulant Therapy: These medications help prevent blood clots and reduce the risk of further complications.
Beta-Blockers and Calcium Channel Blockers: These drugs help lower blood pressure and reduce the strain on the heart.
Percutaneous Coronary Intervention (PCI)
PCI, also known as angioplasty, involves the insertion of a balloon catheter into the narrowed or torn artery. The balloon is inflated to widen the artery, and a stent may be placed to keep the artery open.
Coronary Artery Bypass Grafting (CABG)
In severe cases, surgical intervention may be necessary. CABG involves grafting a healthy blood vessel from another part of the body to bypass the damaged artery, restoring blood flow to the heart.
Lifestyle Modifications
Smoking Cessation: Quitting smoking can significantly reduce the risk of arterial tears and improve overall cardiovascular health.
Diet and Exercise: Adopting a heart-healthy diet and engaging in regular physical activity can help manage risk factors such as high cholesterol, hypertension, and diabetes.
Prevention And Risk Reduction
Preventing arterial tears in the heart involves addressing the underlying risk factors and adopting a proactive approach to cardiovascular health. Here are some strategies for prevention and risk reduction:
Regular Medical Checkups
Routine medical checkups can help identify and manage risk factors such as high blood pressure, high cholesterol, and diabetes. Early detection and treatment of these conditions can reduce the risk of arterial tears.
Healthy Lifestyle Choices
Balanced Diet: A diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats can support cardiovascular health and reduce the risk of atherosclerosis.
Physical Activity: Regular exercise can help maintain a healthy weight, lower blood pressure, and improve overall cardiovascular health.
Stress Management: Practicing stress-reducing techniques such as meditation, yoga, and deep breathing can help manage emotional stress and reduce the risk of arterial tears.
Avoiding Harmful Substances
Avoiding the use of tobacco, recreational drugs, and excessive alcohol can significantly reduce the risk of arterial tears and improve overall cardiovascular health.
Medication Adherence
For individuals with underlying conditions such as SCAD or atherosclerosis, adhering to prescribed medications and following the treatment plan can help manage the condition and reduce the risk of complications.
Conclusion
An arterial tear in the heart is a serious condition that requires immediate medical attention. Understanding the various causes and risk factors is essential for prevention, early detection, and effective treatment. By addressing underlying conditions, adopting a heart-healthy lifestyle, and seeking prompt medical care, individuals can reduce their risk of arterial tears and improve their overall cardiovascular health.