Atrial fibrillation (AF) is the most common sustained cardiac arrhythmia encountered in clinical practice, affecting millions of individuals worldwide. Characterized by disorganized electrical activity in the atria, AF predisposes patients to a heightened risk of stroke, heart failure, and other cardiovascular complications. Management strategies for AF include both pharmacological and non-pharmacological approaches, with medications playing a crucial role in rhythm control, rate control, and stroke prevention. This article aims to provide a comprehensive overview of the five main classes of medications used in the treatment of atrial fibrillation, highlighting their mechanisms of action, efficacy, safety profiles, and clinical indications.
5 Medications Used to Treat Atrial Fibrillation
Class I: Sodium Channel Blockers
Sodium channel blockers are antiarrhythmic drugs that exert their effects by blocking sodium channels in cardiac myocytes, thereby inhibiting fast inward sodium currents responsible for phase 0 depolarization. This class of medications includes agents like flecainide and propafenone, which are commonly used for rhythm control in atrial fibrillation.
SEE ALSO: What Rate Is Considered SVT?
1. Flecainide
Flecainide is a class IC antiarrhythmic drug that works by prolonging the atrial and ventricular refractory periods, thereby preventing reentry of electrical impulses and stabilizing cardiac rhythm. It is indicated for patients with paroxysmal atrial fibrillation and no structural heart disease. Flecainide should be used cautiously in patients with structural heart disease due to the risk of proarrhythmia.
2. Propafenone
Propafenone is another class IC antiarrhythmic agent that exhibits both sodium channel blocking and mild beta-blocking properties. It is effective in converting recent-onset atrial fibrillation to sinus rhythm and is also used for maintenance of sinus rhythm in patients with paroxysmal AF. Like flecainide, propafenone should be used with caution in patients with structural heart disease.
Class II: Beta-Blockers
Beta-blockers are a cornerstone in the management of atrial fibrillation, primarily for rate control rather than rhythm control. They exert their effects by antagonizing beta-adrenergic receptors, thereby reducing sympathetic tone and slowing atrioventricular nodal conduction.
3. Metoprolol
Metoprolol is a selective beta-1 adrenergic receptor blocker that is frequently used in clinical practice for rate control in atrial fibrillation. It reduces heart rate, improves diastolic filling time, and enhances ventricular filling, thereby improving symptoms and preventing tachycardia-induced cardiomyopathy.
4. Atenolol
Atenolol is another beta-1 selective adrenergic blocker that may be used for rate control in atrial fibrillation. Its use, however, has declined in recent years due to concerns over its efficacy profile compared to other beta-blockers such as metoprolol and bisoprolol.
Class III: Potassium Channel Blockers
Potassium channel blockers prolong the action potential duration and effective refractory period in cardiac cells, thereby exerting antiarrhythmic effects. They are particularly useful for maintaining sinus rhythm in patients with persistent atrial fibrillation.
5. Amiodarone
Amiodarone is a broad-spectrum antiarrhythmic drug with potent class III properties, as well as effects on other ion channels (class I, II, and IV). It is highly effective for both rate and rhythm control in atrial fibrillation and is often used when other agents have failed or are contraindicated. However, its use is limited by potential serious adverse effects, including pulmonary toxicity, thyroid dysfunction, and hepatotoxicity.
Class IV: Calcium Channel Blockers
Calcium channel blockers primarily act by inhibiting the influx of calcium ions through L-type calcium channels in cardiac and smooth muscle cells, leading to negative chronotropic and dromotropic effects.
They are used primarily for rate control in atrial fibrillation.
6. Dilti$azem
Diltiazem is a non-dihydropyridine calcium channel blocker that is frequently employed for rate control in atrial fibrillation. It slows atrioventricular nodal conduction, thereby reducing ventricular response rate during atrial fibrillation episodes. Diltiazem is particularly useful in patients with concomitant hypertension or coronary artery disease.
Class V: Anticoagulants: Stroke Prevention in Atrial Fibrillation
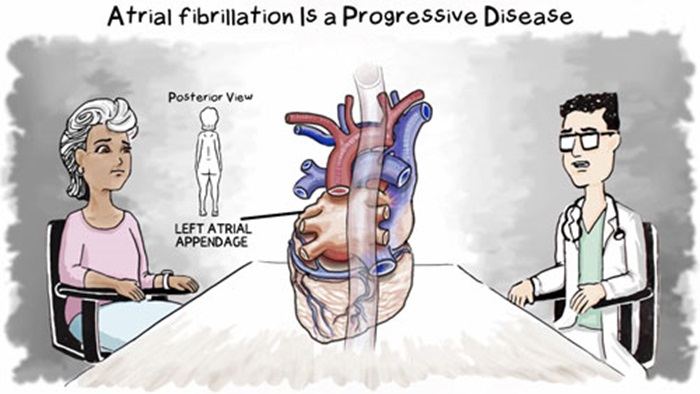
Anticoagulation is a cornerstone in the management of atrial fibrillation to prevent thromboembolic events, particularly ischemic stroke. The risk of stroke in AF is primarily related to the formation of thrombi within the left atrial appendage due to blood stasis. Oral anticoagulants are categorized into vitamin K antagonists (e.g., warfarin) and non-vitamin K antagonist oral anticoagulants (NOACs, e.g., dabigatran, rivaroxaban, apixaban, edoxaban).
Conclusion
In conclusion, the management of atrial fibrillation requires a tailored approach that considers the patient’ssymptoms, comorbidities, and individual risk factors. Pharmacological therapy remains a cornerstone in the treatment of AF, with medications used for rhythm control, rate control, and stroke prevention playing pivotal roles in clinical practice. It is essential for healthcare providers to have a thorough understanding of the mechanisms of action, indications, contraindications, and potential adverse effects associated with each class of medications discussed in this article to optimize patient outcomes and minimize risks. Future research efforts aimed at refining treatment strategies and identifying novel therapeutic targets hold promise for further improving the management of this prevalent cardiac arrhythmia.