Cardiovascular disease remains a leading cause of mortality worldwide, with coronary artery disease (CAD) being a significant contributor. Among the various treatments available for CAD, coronary stenting has become a cornerstone intervention. This article aims to explore in depth why cardiologists choose to implant stents in the heart, discussing the indications, procedure details, types of stents, outcomes, and future directions in stent technology.
Evolution of Coronary Stenting
The development of coronary stenting represents a significant advancement in the field of interventional cardiology. Before stents, balloon angioplasty was the primary method used to open blocked coronary arteries. However, its limitations, such as elastic recoil and acute vessel closure, prompted the need for a more effective solution.
The introduction of bare-metal stents (BMS) in the 1980s revolutionized coronary interventions by providing structural support to keep the artery open post-angioplasty.
SEE ALSO: What New Drugs Will Unclog Arteries in 2024?
Indications for Coronary Stenting
Stable Coronary Artery Disease
Stenting is commonly indicated in stable CAD when symptoms persist despite optimal medical therapy. Symptoms may include angina pectoris or ischemic changes on stress testing, indicating significant coronary artery stenosis. Stenting aims to relieve symptoms and improve exercise tolerance by restoring adequate blood flow to the myocardium.
Acute Coronary Syndrome (ACS)
In ACS, which encompasses unstable angina, non-ST-segment elevation myocardial infarction (NSTEMI), and ST-segment elevation myocardial infarction (STEMI), prompt revascularization is crucial. Stenting plays a vital role in restoring coronary blood flow and limiting myocardial damage, particularly in the setting of STEMI where “time is muscle.”
Post-Interventional Restenosis
Despite advancements, restenosis—re-narrowing of the treated artery—remains a concern after stent placement. Drug-eluting stents (DES), introduced in the early 2000s, have significantly reduced restenosis rates compared to BMS by releasing anti-proliferative drugs that inhibit smooth muscle cell proliferation and reduce neointimal hyperplasia.
Types of Coronary Stents
Bare-Metal Stents (BMS)
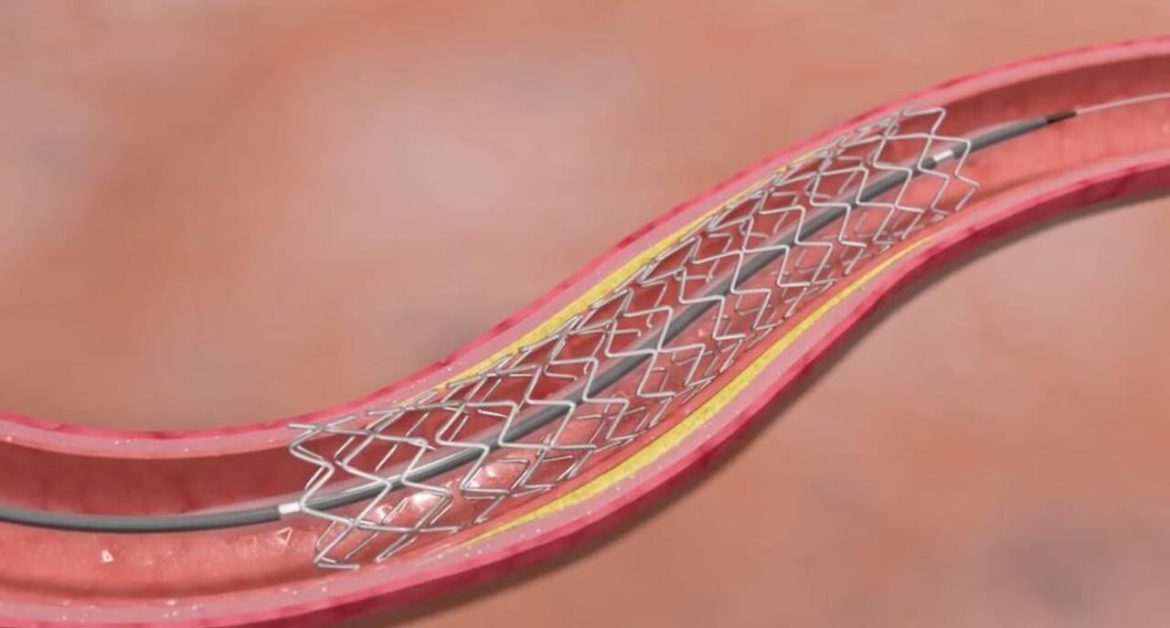
BMS consist of a metal mesh tube (usually stainless steel) that provides mechanical support to the coronary artery. They are effective in reducing acute vessel closure post-angioplasty but are associated with higher rates of restenosis compared to DES.
Drug-Eluting Stents (DES)
DES are coated with a polymer containing anti-proliferative drugs (e.g., sirolimus, paclitaxel) that are released over time to inhibit smooth muscle cell growth. This significantly reduces the risk of restenosis compared to BMS but carries a slightly higher risk of late stent thrombosis, necessitating prolonged dual antiplatelet therapy.
Bioresorbable Vascular Scaffolds (BVS)
BVS are a novel type of stent designed to provide temporary support to the coronary artery while gradually dissolving over time. This concept aims to restore normal vascular physiology and potentially reduce long-term complications associated with permanent metallic implants.
However, early-generation BVS faced challenges such as higher rates of device thrombosis, leading to cautious adoption and ongoing development efforts.
The Coronary Stenting Procedure
Pre-Procedural Assessment
Before coronary stenting, comprehensive assessment is crucial. This includes clinical evaluation, electrocardiography (ECG), echocardiography, and coronary angiography to determine the extent and severity of CAD. Functional testing such as stress testing or fractional flow reserve (FFR) may also be utilized to assess lesion significance and guide treatment decisions.
Interventional Procedure
Coronary stenting is typically performed in a cardiac catheterization laboratory (cath lab) under local anesthesia and conscious sedation.
Using fluoroscopic guidance, a guide catheter is inserted through the femoral or radial artery and advanced to the coronary arteries. A coronary guidewire is then threaded across the lesion, followed by balloon angioplasty to dilate the narrowed segment. Subsequently, the stent is deployed at the lesion site, expanding against the vessel wall and restoring blood flow.
Post-Procedural Care
After stent implantation, patients are monitored closely for complications such as bleeding, contrast-induced nephropathy, and vascular complications at the access site. Dual antiplatelet therapy with aspirin and a P2Y12 inhibitor (e.g., clopidogrel, ticagrelor) is initiated to prevent stent thrombosis, with the duration based on stent type, clinical presentation, and bleeding risk.
Outcomes And Complications
Clinical Outcomes
The primary goal of coronary stenting is to alleviate symptoms and improve quality of life in patients with CAD. Clinical outcomes are generally favorable, with significant reductions in angina frequency and improvements in exercise tolerance observed post-stenting. Moreover, timely revascularization in ACS can reduce mortality and morbidity associated with myocardial infarction.
Complications
Despite advancements in stent technology and procedural techniques, complications can occur. These include stent thrombosis (acute or late), in-stent restenosis, contrast-induced nephropathy, access site complications, and bleeding.
Strategies to mitigate these risks include appropriate patient selection, meticulous procedural technique, and optimized post-procedural care.
Future Directions in Stent Technology
Bioengineering Innovations
Ongoing research focuses on developing stents with improved biocompatibility and reduced risk of long-term complications.
Bioresorbable stents, in particular, aim to provide temporary scaffolding while promoting vascular healing and minimizing late adverse events associated with permanent implants.
Drug Delivery Systems
Advancements in drug-eluting technologies aim to enhance drug delivery efficiency and safety profiles. Novel drugs and coatings are under investigation to further reduce neointimal hyperplasia while minimizing the risk of delayed healing or thrombosis.
Imaging And Physiology-Guided Interventions
Integration of intravascular imaging (e.g., intravascular ultrasound, optical coherence tomography) and physiological assessments (e.g., FFR, instantaneous wave-free ratio) enhances procedural precision by providing detailed information on plaque morphology, stent deployment, and post-procedural optimization.
Personalized Medicine Approaches
Tailoring treatment strategies based on individual patient characteristics, genetic profiles, and lesion characteristics may optimize outcomes and reduce adverse events. Precision medicine initiatives seek to refine risk stratification algorithms and therapeutic interventions in coronary stenting.
Conclusion
Coronary stenting represents a cornerstone in the management of CAD, offering effective relief of symptoms and improvement in clinical outcomes for patients with coronary artery stenosis. Advances in stent technology, from bare-metal to drug-eluting and bioresorbable stents, have significantly enhanced procedural success rates and long-term efficacy.
Ongoing research continues to refine stent design, drug delivery systems, and procedural techniques to further improve patient outcomes and minimize complications associated with coronary interventions.