Myocarditis, an inflammation of the heart muscle (myocardium), is a condition that can significantly impact cardiac function and overall health. While it is often associated with abnormal findings on an electrocardiogram (ECG), it is possible for myocarditis to present with a normal ECG. This phenomenon can complicate the diagnosis and management of the condition. In this article, we will explore the intricacies of myocarditis, the role of ECG in its diagnosis, and the implications of a normal ECG in patients with myocarditis.
Understanding Myocarditis
Definition and Etiology
Myocarditis refers to inflammation of the myocardium, the middle layer of the heart wall responsible for contracting and pumping blood. This inflammation can result from various causes, including:
Viral Infections: Commonly caused by enteroviruses, adenoviruses, and the recent SARS-CoV-2 (COVID-19).
Bacterial Infections: Such as diphtheria and Lyme disease.
Fungal and Parasitic Infections: Rare, but include infections like Chagas disease.
Autoimmune Diseases: Conditions like systemic lupus erythematosus and rheumatoid arthritis.
Toxins and Drugs: Including certain chemotherapy agents and excessive alcohol consumption.
SEE ALSO: 8 Diseases Are Easily Misdiagnosed as Myocarditis?
Pathophysiology
The inflammatory process in myocarditis can lead to myocardial cell damage, necrosis, and subsequent fibrosis. This can impair the heart’s ability to contract efficiently, potentially resulting in heart failure, arrhythmias, or cardiogenic shock. The extent and severity of inflammation can vary widely, influencing the clinical presentation and prognosis.
Clinical Presentation of Myocarditis
The symptoms of myocarditis can be highly variable, ranging from mild, nonspecific complaints to severe, life-threatening conditions.
Common symptoms include:
Chest Pain: Often sharp and pleuritic, resembling pericarditis.
Fatigue and Dyspnea: Due to reduced cardiac output and heart failure.
Palpitations: Resulting from arrhythmias.
Syncope: Caused by severe arrhythmias or heart failure.
Flu-like Symptoms: Fever, myalgia, and sore throat in cases of viral myocarditis.
Given this broad spectrum of symptoms, the diagnosis of myocarditis can be challenging and often requires a high index of suspicion.
Diagnostic Tools for Myocarditis
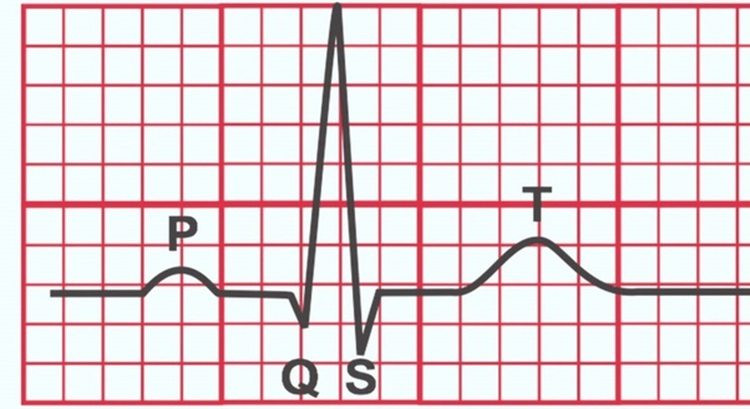
Electrocardiogram (ECG)
The ECG is a readily available, non-invasive tool commonly used to evaluate patients with suspected myocarditis. Typical ECG findings in myocarditis may include:
ST-segment Elevation or Depression: Indicative of myocardial injury or pericarditis.
T-wave Inversion: Reflecting myocardial inflammation or ischemia.
Arrhythmias: Such as atrial or ventricular tachycardia, or premature ventricular contractions.
Low Voltage QRS Complexes: Due to myocardial edema or pericardial effusion.
However, these findings are not specific to myocarditis and can be seen in various other cardiac conditions. Importantly, the ECG can be normal in some patients with myocarditis, particularly in early or mild cases.
Cardiac Biomarkers
Elevated levels of cardiac biomarkers, such as troponins and creatine kinase-MB (CK-MB), can indicate myocardial injury and support the diagnosis of myocarditis. However, these markers are not always elevated, especially in mild or subclinical cases.
Imaging Studies
Echocardiography: Can reveal wall motion abnormalities, reduced ejection fraction, or pericardial effusion, but may be normal in early or mild myocarditis.
Cardiac Magnetic Resonance Imaging (MRI): The gold standard for diagnosing myocarditis. It can detect myocardial edema, hyperemia, and late gadolinium enhancement, which are indicative of inflammation and fibrosis.
Endomyocardial Biopsy: The definitive diagnostic tool, though invasive and not routinely performed. It allows for histopathological confirmation of myocarditis.
Myocarditis with Normal ECG: Possible Scenarios
Early or Mild Myocarditis
In the early stages of myocarditis, the inflammatory process may not be extensive enough to produce significant changes on the ECG.
Similarly, in cases of mild myocarditis, the degree of myocardial inflammation may be insufficient to disrupt the electrical activity of the heart, resulting in a normal ECG.
Focal Myocarditis
Myocarditis can be focal, affecting only small areas of the myocardium. If these areas do not involve the regions that predominantly influence the ECG, such as the septum or the anterior wall, the ECG may appear normal despite ongoing inflammation.
Subclinical Myocarditis
Subclinical myocarditis refers to inflammation that does not produce overt symptoms or significant myocardial injury. This form of myocarditis may not manifest any ECG abnormalities, making it particularly challenging to diagnose without advanced imaging techniques like cardiac MRI.
False-Negative ECG
The sensitivity of the ECG in detecting myocarditis is not absolute.
Certain ECG abnormalities may be transient or subtle, potentially leading to false-negative results. Repeating the ECG or employing continuous monitoring (e.g., Holter monitoring) may sometimes reveal transient arrhythmias or other abnormalities missed on a standard ECG.
Clinical Implications And Management
Diagnostic Challenges
A normal ECG in a patient with suspected myocarditis necessitates a careful and comprehensive evaluation. Relying solely on the ECG can lead to missed diagnoses and delayed treatment. Clinicians should consider other diagnostic modalities, such as cardiac biomarkers and advanced imaging techniques, to confirm or exclude myocarditis.
Risk Stratification
Patients with myocarditis and a normal ECG may still be at risk for complications. It is essential to assess other clinical parameters, such as the presence of symptoms, cardiac biomarkers, and imaging findings, to determine the severity of the condition and guide management decisions.
Treatment Approach
The treatment of myocarditis is primarily supportive and tailored to the severity of the condition:
Mild Cases: May require rest and symptomatic treatment, including nonsteroidal anti-inflammatory drugs (NSAIDs) for pain relief.
Moderate to Severe Cases: May necessitate hospitalization, especially if heart failure or arrhythmias are present. Treatment may include diuretics, ACE inhibitors, beta-blockers, or antiarrhythmic medications.
Fulminant Myocarditis: Characterized by severe heart failure and cardiogenic shock, requiring intensive care management, including inotropic support, mechanical ventilation, or extracorporeal membrane oxygenation (ECMO).
Monitoring and Follow-Up
Patients with myocarditis, regardless of ECG findings, require close follow-up to monitor for resolution of inflammation and recovery of cardiac function. Serial imaging and biomarker assessment may be necessary to guide the duration of treatment and determine the need for long-term management.
Conclusion
Can You Have Myocarditis with Normal ECG?
The answer is yes. Myocarditis can indeed present with a normal ECG, particularly in early, mild, focal, or subclinical cases.
While the ECG remains a valuable tool in the initial evaluation of myocarditis, it is not definitive. A normal ECG does not exclude myocarditis, and clinicians should employ a multi-modal diagnostic approach, including cardiac biomarkers and advanced imaging, to ensure accurate diagnosis and appropriate management.