The COVID-19 pandemic has significantly impacted global health, presenting various complications that affect multiple organ systems. Among these, myocarditis—a condition characterized by inflammation of the heart muscle—has emerged as a notable cardiovascular complication associated with SARS-CoV-2 infection. Diagnosing COVID-19 myocarditis requires a comprehensive understanding of its clinical presentation, diagnostic tools, and differential diagnosis.
How to Diagnose COVID-19 Myocarditis
1. Clinical Presentation and Initial Assessment
COVID-19 myocarditis can present with a wide range of symptoms, from mild to severe. Patients may experience chest pain, palpitations, shortness of breath, and fatigue. In severe cases, signs of heart failure, cardiogenic shock, or arrhythmias may be evident. Given the overlap of symptoms with other cardiovascular and respiratory conditions, a high index of suspicion is necessary, particularly in COVID-19 patients presenting with cardiac symptoms.
History and Physical Examination: A thorough patient history and physical examination are crucial initial steps. Key points to inquire about include recent COVID-19 infection or exposure, onset and nature of cardiac symptoms, and any history of cardiovascular disease. Physical examination may reveal signs of heart failure such as elevated jugular venous pressure, peripheral edema, and crackles on lung auscultation.
SEE ALSO: Does Myocarditis Cause Slow Heart Rate?
2. Laboratory Tests
Laboratory tests play a significant role in the diagnostic process. Key biomarkers indicative of myocardial injury and inflammation should be assessed.
Troponin: Elevated troponin levels are a hallmark of myocardial injury. In COVID-19 patients, elevated troponin may indicate myocarditis, though it is not specific and can also be seen in other cardiac and non-cardiac conditions.
B-type Natriuretic Peptide (BNP) or N-terminal pro-BNP (NT-proBNP): These markers are elevated in cases of heart failure and can help assess the severity of cardiac dysfunction.
C-Reactive Protein (CRP) and Erythrocyte Sedimentation Rate (ESR): Elevated inflammatory markers like CRP and ESR suggest systemic inflammation, which is common in COVID-19 myocarditis.
3. Imaging Studies
Imaging studies are essential for assessing cardiac structure and function, as well as detecting inflammatory changes.
Echocardiography: Echocardiography is a readily available, non-invasive tool that provides valuable information on cardiac function and structure. Findings suggestive of myocarditis include left ventricular dysfunction, wall motion abnormalities, and pericardial effusion. Speckle-tracking echocardiography can further assess myocardial strain and detect subtle changes in myocardial function.
Cardiac Magnetic Resonance Imaging (CMR): CMR is considered the gold standard for diagnosing myocarditis. It provides detailed tissue characterization and can identify myocardial edema, hyperemia, and fibrosis. Late gadolinium enhancement (LGE) is particularly useful for detecting myocardial scarring, a key feature of myocarditis. CMR can also exclude other causes of myocardial injury.
4. Electrocardiography (ECG)
ECG: An ECG should be performed in all patients with suspected myocarditis. Common findings in COVID-19 myocarditis include ST-segment changes, T-wave inversions, and conduction abnormalities. However, these findings are non-specific and must be interpreted in conjunction with clinical and other diagnostic data.
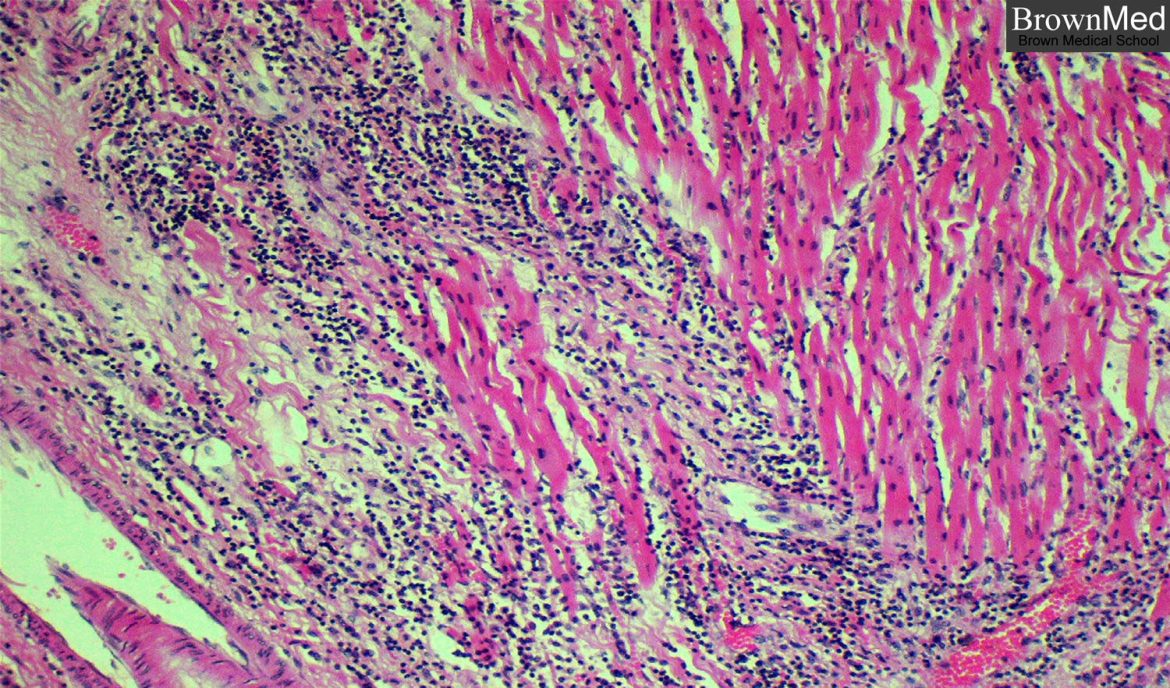
5. Endomyocardial Biopsy (EMB)
Endomyocardial Biopsy: EMB remains the definitive diagnostic tool for myocarditis, providing histopathological evidence of inflammation and myocardial injury. However, its invasive nature and potential complications limit its use to select cases where non-invasive methods are inconclusive, and the diagnosis is critical for management decisions.
Differential Diagnosis
Differentiating COVID-19 myocarditis from other conditions with similar presentations is essential.
Acute Coronary Syndrome (ACS): ACS can present with elevated troponin levels and similar symptoms. Coronary angiography may be necessary to exclude obstructive coronary artery disease.
Pericarditis: Pericarditis can coexist with or mimic myocarditis. Distinguishing features include pericardial friction rub and diffuse ST-segment elevation on ECG. Cardiac MRI can help differentiate between the two conditions.
Heart Failure: COVID-19 can exacerbate pre-existing heart failure or cause new-onset heart failure. Echocardiography and biomarkers (BNP, NT-proBNP) are useful in assessing heart failure.
Other Viral Myocarditis: Myocarditis can be caused by various viruses. Serological tests and viral PCR may help identify other viral etiologies.
Emerging Diagnostic Tools
Positron Emission Tomography (PET): PET imaging, particularly with 18F-fluorodeoxyglucose (FDG), can identify areas of myocardial inflammation. Its role in diagnosing COVID-19 myocarditis is still being explored.
Artificial Intelligence (AI): AI and machine learning algorithms are being developed to enhance the accuracy of diagnostic tools, particularly in imaging studies.
Case Management And Follow-up
Once COVID-19 myocarditis is diagnosed, appropriate management and follow-up are crucial to ensure optimal outcomes.
Management:
Supportive Care: Patients with COVID-19 myocarditis should receive standard care for heart failure, including diuretics, ACE inhibitors, beta-blockers, and other guideline-directed medical therapies.
Anti-inflammatory Therapy: In selected cases, particularly those with severe myocarditis, immunosuppressive therapy (e.g., corticosteroids, intravenous immunoglobulin) may be considered. However, the use of these therapies remains controversial and should be based on individual patient characteristics and expert consultation.
Antiviral Treatment: Specific antiviral treatments for COVID-19, such as remdesivir, may be considered as part of the overall management strategy, especially in the early phase of the disease.
Arrhythmia Management: Arrhythmias are common in myocarditis and may require specific antiarrhythmic therapy or device implantation (e.g., pacemakers, implantable cardioverter-defibrillators) in severe cases.
Hemodynamic Support: In cases of cardiogenic shock, advanced hemodynamic support with inotropes, vasopressors, or mechanical circulatory support (e.g., intra-aortic balloon pump, extracorporeal membrane oxygenation) may be necessary.
Conclusion
Diagnosing COVID-19 myocarditis requires a multifaceted approach that includes clinical evaluation, laboratory tests, imaging studies, and, in select cases, endomyocardial biopsy. Given the potential for significant morbidity and mortality, early recognition and appropriate management are critical. Continued research and advancements in diagnostic tools will further enhance our ability to diagnose and treat this complex condition, ultimately improving patient outcomes.