Cardiogenic cirrhosis, also known as cardiac cirrhosis or congestive hepatopathy, is a liver disorder that arises due to chronic cardiac dysfunction. The liver, being a highly vascular organ, is particularly susceptible to the effects of prolonged cardiac insufficiency. Understanding the underlying causes of cardiogenic cirrhosis is crucial for cardiologists and hepatologists in providing effective management and treatment. In this article, we will explore the five primary causes of cardiogenic cirrhosis.
5 Causes of Cardiogenic Cirrhosis
1. Chronic Heart Failure
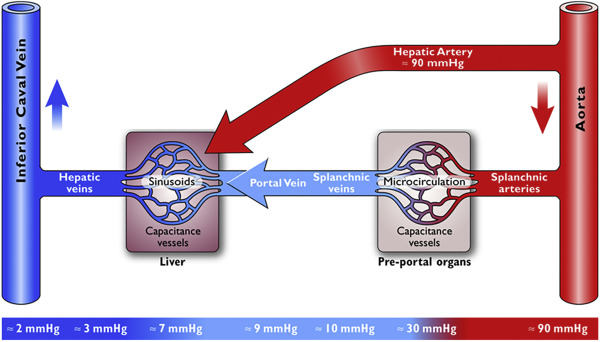
Chronic heart failure (CHF) is a major cause of cardiogenic cirrhosis. When the heart is unable to pump blood efficiently, it leads to increased pressure in the central venous system, particularly in the inferior vena cava and hepatic veins. This elevated pressure is transmitted to the liver, resulting in congestion and subsequent liver damage. Over time, the sustained hepatic congestion impairs liver function, causing hepatocyte necrosis and fibrosis, ultimately leading to cirrhosis.
In CHF, the decreased cardiac output reduces perfusion to vital organs, including the liver. This hypoperfusion, combined with congestion, exacerbates liver injury. The pathophysiology involves both backward failure (increased venous pressure) and forward failure (decreased arterial perfusion), creating a dual mechanism of liver damage. Management of CHF through medications such as diuretics, beta-blockers, and ACE inhibitors, along with lifestyle modifications, can help mitigate the progression of cardiogenic cirrhosis.
SEE ALSO: What Two Symptoms Do Babies with Heart Disease Usually Have
2. Constrictive Pericarditis
Constrictive pericarditis is a condition where the pericardium, the fibrous sac surrounding the heart, becomes thickened and scarred, restricting the heart’s normal movement and function. This restriction leads to impaired ventricular filling, elevated central venous pressure, and subsequent hepatic congestion. The prolonged congestion causes sinusoidal dilatation and perisinusoidal fibrosis in the liver, eventually resulting in cirrhosis.
The liver in patients with constrictive pericarditis often shows signs of chronic passive congestion, including the classic “nutmeg liver” appearance on histology. Surgical intervention, such as pericardiectomy, is often required to relieve the pericardial constriction and alleviate the hepatic congestion. Early diagnosis and treatment are essential to prevent irreversible liver damage and the progression to cirrhosis.
3. Tricuspid Valve Disease
Tricuspid valve disease, particularly tricuspid regurgitation, significantly contributes to the development of cardiogenic cirrhosis. Tricuspid regurgitation leads to the backflow of blood from the right ventricle into the right atrium during systole, resulting in increased right atrial pressure and hepatic venous congestion. The liver, subjected to chronic venous hypertension, undergoes structural changes, including fibrosis and cirrhosis.
Tricuspid valve disease can be congenital or acquired, often secondary to conditions such as rheumatic heart disease, infective endocarditis, or carcinoid syndrome. Treatment options include medical management to reduce symptoms and surgical interventions, such as valve repair or replacement, to correct the underlying valve pathology. Addressing tricuspid valve disease can significantly improve hepatic congestion and prevent the progression to cirrhosis.
4. Cor Pulmonale
Cor pulmonale, or right-sided heart failure due to pulmonary hypertension, is another significant cause of cardiogenic cirrhosis. Pulmonary hypertension, often secondary to chronic lung diseases such as chronic obstructive pulmonary disease (COPD) or pulmonary embolism, increases the workload on the right ventricle, leading to right ventricular hypertrophy and failure. The elevated pressure in the right side of the heart is transmitted back to the hepatic veins, causing congestion and liver damage.
Patients with cor pulmonale may present with symptoms of both cardiac and respiratory failure, complicating the clinical picture. Effective management of the underlying pulmonary condition, along with supportive cardiac therapies, is essential to reduce hepatic congestion and prevent cirrhosis. In severe cases, advanced therapies such as lung transplantation or pulmonary artery hypertension-targeted treatments may be considered.
5. Congenital Heart Diseases
Certain congenital heart diseases, such as Ebstein’s anomaly, Eisenmenger syndrome, and congenital tricuspid atresia, predispose patients to cardiogenic cirrhosis. These conditions often involve structural abnormalities that lead to chronic right-sided heart failure and subsequent hepatic congestion. The prolonged elevated venous pressure causes progressive liver damage and fibrosis, eventually resulting in cirrhosis.
In congenital heart diseases, early diagnosis and appropriate surgical or interventional treatments are crucial to prevent complications, including cardiogenic cirrhosis.
In some cases, palliative measures may be necessary to manage symptoms and improve quality of life. Regular monitoring of liver function and early intervention in cases of hepatic decompensation are essential components of managing these patients.
Conclusion
Cardiogenic cirrhosis is a serious complication arising from chronic cardiac conditions that lead to hepatic congestion and subsequent liver damage. Understanding the underlying causes, such as chronic heart failure, constrictive pericarditis, tricuspid valve disease, cor pulmonale, and congenital heart diseases, is vital for effective management and prevention.
Early diagnosis and treatment of the cardiac conditions, along with vigilant monitoring of liver function, can significantly improve outcomes and quality of life for affected patients. As cardiologists, a comprehensive approach that addresses both cardiac and hepatic health is essential in managing cardiogenic cirrhosis.