Cardiomyopathy is a condition characterized by the abnormal functioning of the heart muscle. This disease can lead to serious health issues, including heart failure, arrhythmias, and sudden cardiac death. Understanding the causes of cardiomyopathy is crucial for early diagnosis, effective treatment, and prevention. In this article, we will delve into the various factors that contribute to the development of cardiomyopathy, highlighting genetic, environmental, and lifestyle influences.
1. Genetic Factors
Genetics play a significant role in the development of cardiomyopathy. Many forms of the disease are hereditary, passed down through families. There are several types of cardiomyopathy, each associated with specific genetic mutations.
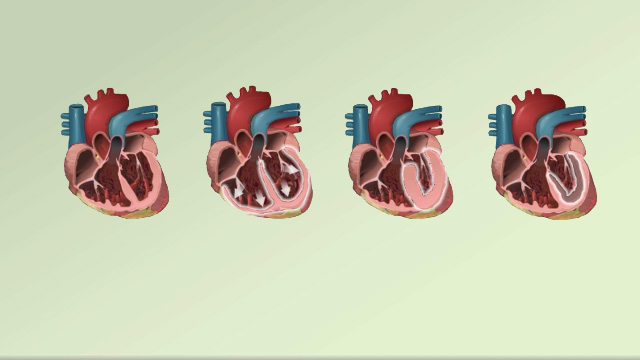
Hypertrophic Cardiomyopathy (HCM)
Hypertrophic cardiomyopathy is often caused by mutations in genes that encode proteins in the heart muscle. These mutations lead to the thickening of the heart muscle, particularly the septum between the ventricles. Common genes involved include MYH7, MYBPC3, TNNT2, and TNNI3. These genetic alterations result in the abnormal arrangement of muscle fibers, known as myofibrillar disarray, which impairs the heart’s ability to pump blood efficiently.
see also:What Happens When A Heart Stent Fails
Dilated Cardiomyopathy (DCM)
Dilated cardiomyopathy is characterized by the enlargement and weakening of the heart chambers, leading to reduced pumping efficiency. Genetic mutations are responsible for approximately 30-40% of DCM cases. Mutations in genes such as TTN, LMNA, and SCN5A have been identified as common culprits. These genes are involved in the structure and function of cardiac muscle cells, and their alteration can disrupt normal heart function.
Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC)
Arrhythmogenic right ventricular cardiomyopathy is a condition where the heart muscle is replaced by fatty and fibrous tissue, predominantly in the right ventricle. This can lead to arrhythmias and sudden cardiac death. ARVC is often caused by mutations in genes encoding desmosomal proteins, which are responsible for cell-to-cell adhesion in the heart muscle. Key genes include PKP2, DSP, and DSG2.
Restrictive Cardiomyopathy (RCM)
Restrictive cardiomyopathy is less common but can be genetically influenced. It is characterized by the stiffening of the heart muscle, which restricts its ability to fill with blood. Mutations in genes such as TNNI3 and MYH7 can lead to RCM.
These mutations affect the proteins that regulate muscle contraction, leading to impaired cardiac function.
2. Environmental Factors
While genetics play a significant role, environmental factors can also contribute to the development of cardiomyopathy.
These factors can act independently or in conjunction with genetic predispositions to exacerbate the condition.
Infections
Viral infections, such as myocarditis, can damage the heart muscle and lead to cardiomyopathy. Coxsackievirus, adenovirus, and parvovirus B19 are among the common viruses associated with myocarditis. The infection triggers an inflammatory response, causing damage to the heart muscle cells and leading to dilated cardiomyopathy in severe cases.
Toxins and Alcohol
Exposure to certain toxins, including heavy metals like lead and mercury, can damage the heart muscle. Chronic alcohol abuse is a well-known cause of dilated cardiomyopathy, often referred to as alcoholic cardiomyopathy. Alcohol has a direct toxic effect on the heart muscle cells, leading to their weakening and enlargement.
Medications and Chemotherapy
Certain medications and chemotherapy agents can have cardiotoxic effects. Anthracyclines, a class of chemotherapy drugs, are particularly notorious for causing dilated cardiomyopathy. Other drugs, such as some antipsychotics and immunosuppressants, can also contribute to heart muscle damage.
Nutritional Deficiencies
Nutritional deficiencies, particularly of essential vitamins and minerals, can impact heart health. For example, a deficiency in thiamine (vitamin B1) can lead to a condition known as beriberi, which is associated with dilated cardiomyopathy.
Adequate nutrition is crucial for maintaining the structural and functional integrity of the heart muscle.
3. Lifestyle Factors
Lifestyle choices and behaviors significantly influence the risk of developing cardiomyopathy. These factors are often modifiable, providing opportunities for prevention and management.
Diet and Obesity
A diet high in saturated fats, trans fats, and cholesterol can lead to the buildup of fatty deposits in the arteries, increasing the risk of ischemic cardiomyopathy. Obesity itself is a risk factor for cardiomyopathy, as excess body weight places additional strain on the heart, leading to hypertrophy and eventual heart failure.
Physical Inactivity
A sedentary lifestyle can contribute to the development of cardiomyopathy. Regular physical activity is essential for maintaining cardiovascular health. Lack of exercise can lead to obesity, hypertension, and other risk factors associated with cardiomyopathy.
Smoking
Smoking is a significant risk factor for cardiovascular diseases, including cardiomyopathy. The chemicals in tobacco smoke can damage the heart muscle and blood vessels, leading to ischemic cardiomyopathy. Quitting smoking is one of the most effective measures to reduce the risk of developing cardiomyopathy.
Alcohol Consumption
Moderate alcohol consumption may have some cardiovascular benefits, but excessive drinking is harmful. Chronic alcohol abuse can lead to alcoholic cardiomyopathy, characterized by the weakening and enlargement of the heart muscle. Limiting alcohol intake is crucial for preventing this form of cardiomyopathy.
Systemic Diseases
Systemic diseases and conditions can also contribute to the development of cardiomyopathy. These diseases often have widespread effects on the body, including the heart.
Diabetes
Diabetes is a significant risk factor for cardiomyopathy. High blood sugar levels can damage the blood vessels and the heart muscle itself. Diabetic cardiomyopathy is characterized by left ventricular hypertrophy and diastolic dysfunction. Managing blood sugar levels through diet, exercise, and medication is crucial for preventing diabetes-related cardiomyopathy.
Hypertension
Chronic high blood pressure (hypertension) forces the heart to work harder to pump blood, leading to hypertrophy of the heart muscle. Over time, this increased workload can result in hypertensive cardiomyopathy, characterized by thickened and stiff heart muscle. Controlling blood pressure through lifestyle changes and medication is essential for preventing this condition.
Autoimmune Diseases
Autoimmune diseases, such as systemic lupus erythematosus (SLE) and rheumatoid arthritis, can affect the heart.
Inflammatory processes associated with these diseases can damage the heart muscle and lead to cardiomyopathy. Managing inflammation through medications and lifestyle modifications is crucial for reducing the risk.
4. Unknown Causes
In some cases, the cause of cardiomyopathy remains unknown. This is referred to as idiopathic cardiomyopathy. Despite extensive testing, no specific genetic, environmental, or lifestyle factors can be identified as the cause. Research is ongoing to uncover potential underlying mechanisms and risk factors for idiopathic cardiomyopathy.
Conclusion
Cardiomyopathy is a complex and multifactorial disease with a variety of genetic, environmental, and lifestyle causes.
Understanding these causes is essential for early diagnosis, effective treatment, and prevention. Genetic factors play a significant role, with specific mutations linked to different types of cardiomyopathy. Environmental factors, including infections, toxins, and medications, can also contribute to the disease. Lifestyle choices, such as diet, physical activity, and smoking, significantly influence the risk of developing cardiomyopathy. Systemic diseases, such as diabetes and hypertension, further exacerbate the condition. In some cases, the cause remains unknown, highlighting the need for continued research. By addressing these factors, individuals can reduce their risk and manage the condition more effectively, improving overall heart health and quality of life.