Coronary artery calcification (CAC) is a prevalent condition in cardiovascular medicine, often indicative of atherosclerotic plaque buildup within the coronary arteries. This process involves the deposition of calcium phosphate minerals in the arterial walls, which can lead to a variety of clinical complications, including the increased risk of myocardial infarction and other cardiovascular events. As a cardiologist, my research delves into the mechanisms, diagnosis, and management of calcified coronary lesions, aiming to provide comprehensive insights for better clinical outcomes.
What Is Coronary Artery Calcification?
Coronary artery calcification refers to the accumulation of calcium deposits in the coronary arteries, which supply blood to the heart muscle. These deposits are a hallmark of atherosclerosis, a chronic inflammatory condition characterized by the buildup of plaques composed of lipids, fibrous tissue, and calcified material. Calcification can occur at various stages of plaque development, contributing to plaque stability or instability, and influencing the clinical presentation of coronary artery disease (CAD).
SEE ALSO: What Causes A Tear in The Heart Artery
Pathophysiology of Coronary Artery Calcification
The pathogenesis of CAC involves complex biological processes, including lipid accumulation, inflammation, and the differentiation of vascular smooth muscle cells into osteoblast-like cells. These processes are influenced by factors such as oxidative stress, metabolic disorders, and genetic predisposition. Calcified plaques can either be stable, reducing the risk of plaque rupture, or unstable, increasing the likelihood of acute coronary syndromes.
Risk Factors for Coronary Artery Calcification
Several risk factors contribute to the development and progression of CAC, including:
Age: The prevalence of CAC increases with age.
Sex: Men are generally at higher risk, though post-menopausal women catch up in prevalence.
Hypertension: High blood pressure accelerates arterial damage and calcification.
Hyperlipidemia: Elevated levels of LDL cholesterol and low levels of HDL cholesterol promote atherosclerosis.
Diabetes Mellitus: Diabetes is a significant risk factor for both the initiation and progression of CAC.
Smoking: Tobacco use is a major risk factor for cardiovascular diseases, including CAC.
Chronic Kidney Disease: Impaired renal function is associated with abnormal calcium-phosphate metabolism, contributing to vascular calcification.
Diagnosis of Coronary Artery Calcification
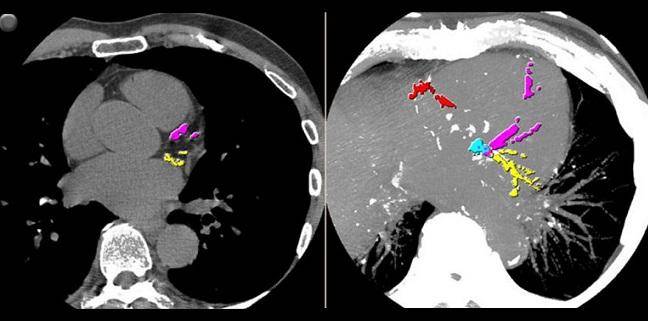
The primary method for diagnosing CAC is through imaging techniques, with the coronary artery calcium score (CACS) being a widely used quantitative measure obtained from non-contrast cardiac computed tomography (CT). The CACS provides a numerical value reflecting the extent of calcification and helps stratify patients’ risk for future cardiovascular events.
Coronary Artery Calcium Score (CACS): A CACS of 0 indicates no detectable calcification, while higher scores indicate increasing amounts of calcium and correspondingly higher risk.
CT Angiography (CTA): Provides detailed images of the coronary arteries and can visualize both calcified and non-calcified plaques.
Intravascular Ultrasound (IVUS) and Optical Coherence Tomography (OCT): These invasive techniques offer high-resolution images of the arterial wall, allowing for the assessment of plaque composition and structure.
Clinical Implications of Calcified Coronary Lesions
Calcified coronary lesions present unique challenges in the management of CAD. The presence of calcification can affect the choice and efficacy of therapeutic interventions, including percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG).
Impact on Percutaneous Coronary Intervention (PCI): Calcified lesions can make balloon angioplasty and stent deployment more difficult, increasing the risk of procedural complications such as stent under-expansion or restenosis. Specialized techniques, such as rotational atherectomy and orbital atherectomy, may be employed to modify calcified plaques and facilitate stent placement.
Impact on Coronary Artery Bypass Grafting (CABG): Extensive calcification of the coronary arteries can complicate surgical revascularization, necessitating alternative grafting strategies or the use of off-pump techniques.
Management of Coronary Artery Calcification
Effective management of CAC involves both pharmacological and non-pharmacological approaches aimed at mitigating risk factors, stabilizing plaques, and improving cardiovascular outcomes.
Pharmacological Interventions
Statins: Statins are the cornerstone of lipid-lowering therapy, reducing LDL cholesterol levels and exerting anti-inflammatory effects. They have been shown to slow the progression of CAC and reduce cardiovascular events.
Antihypertensive Agents: Controlling blood pressure is crucial in reducing the risk of CAC progression and associated complications. ACE inhibitors, ARBs, and calcium channel blockers are commonly used.
Antiplatelet Therapy: Aspirin and other antiplatelet agents help prevent thrombus formation on calcified plaques, reducing the risk of acute coronary syndromes.
Diabetes Management: Strict glycemic control using medications like metformin, SGLT2 inhibitors, and GLP-1 receptor agonists can slow the progression of CAC in diabetic patients.
Non-Pharmacological Interventions
Lifestyle Modifications: Diet, exercise, and smoking cessation are critical components of CAC management. A heart-healthy diet rich in fruits, vegetables, whole grains, and lean proteins can help control cholesterol levels and reduce inflammation.
Regular physical activity improves cardiovascular health, while smoking cessation reduces the risk of atherosclerosis and CAC.
Weight Management: Maintaining a healthy weight through diet and exercise helps reduce the burden of cardiovascular risk factors, including hypertension, hyperlipidemia, and diabetes.
Advanced Therapeutic Techniques
Coronary Atherectomy: Techniques like rotational and orbital atherectomy are employed to modify and debulk heavily calcified plaques, facilitating stent placement and improving procedural outcomes.
Intravascular Lithotripsy (IVL): A novel technique using sonic pressure waves to fracture calcium within the arterial wall, making it easier to expand balloons and deploy stents in calcified lesions.
Future Directions in Coronary Artery Calcification Research
Ongoing research is focused on elucidating the molecular mechanisms underlying CAC, developing novel imaging modalities, and exploring new therapeutic targets. Advances in genetic and biomarker studies hold promise for better risk stratification and personalized treatment approaches.
Molecular and Genetic Insights: Understanding the genetic predisposition and molecular pathways involved in CAC could lead to the identification of novel therapeutic targets and preventive strategies.
Imaging Advances: The development of advanced imaging techniques, such as hybrid PET/CT and molecular imaging, may provide more detailed insights into plaque composition and activity, enhancing risk assessment and treatment planning.
Targeted Therapies: Research into targeted therapies, including anti-inflammatory agents, calcification inhibitors, and regenerative therapies, aims to address the underlying pathological processes of CAC more effectively.
Conclusion
Coronary artery calcification is a significant marker of atherosclerosis and cardiovascular risk, posing challenges for diagnosis and management. Understanding the pathophysiology, risk factors, and clinical implications of calcified coronary lesions is crucial for developing effective treatment strategies. Ongoing research and advances in imaging and therapeutic techniques hold promise for improving outcomes for patients with CAC. As we continue to unravel the complexities of this condition, a multidisciplinary approach encompassing lifestyle modifications, pharmacological interventions, and advanced procedural techniques will be essential in mitigating the impact of coronary artery calcification on cardiovascular health.