Left-sided heart failure, a condition where the left ventricle of the heart is unable to pump blood effectively, leads to a cascade of physiological consequences that primarily affect the lungs and systemic circulation. Understanding the backward effects of left-sided heart failure is crucial for comprehending its impact on the body’s overall function and the symptoms experienced by affected individuals.
Introduction
Left-sided heart failure (LHF) is a prevalent cardiovascular disorder characterized by the heart’s inability to adequately pump blood from the left ventricle to the body’s systemic circulation. This condition often results from underlying cardiovascular diseases such as coronary artery disease, hypertension, or valvular heart disease. As LHF progresses, it manifests through various backward effects, which significantly impact both pulmonary and systemic circulation dynamics.
SEE ALSO: 5 Causes of Cardiogenic Cirrhosis
Anatomy And Physiology of Left-Sided Heart Failure
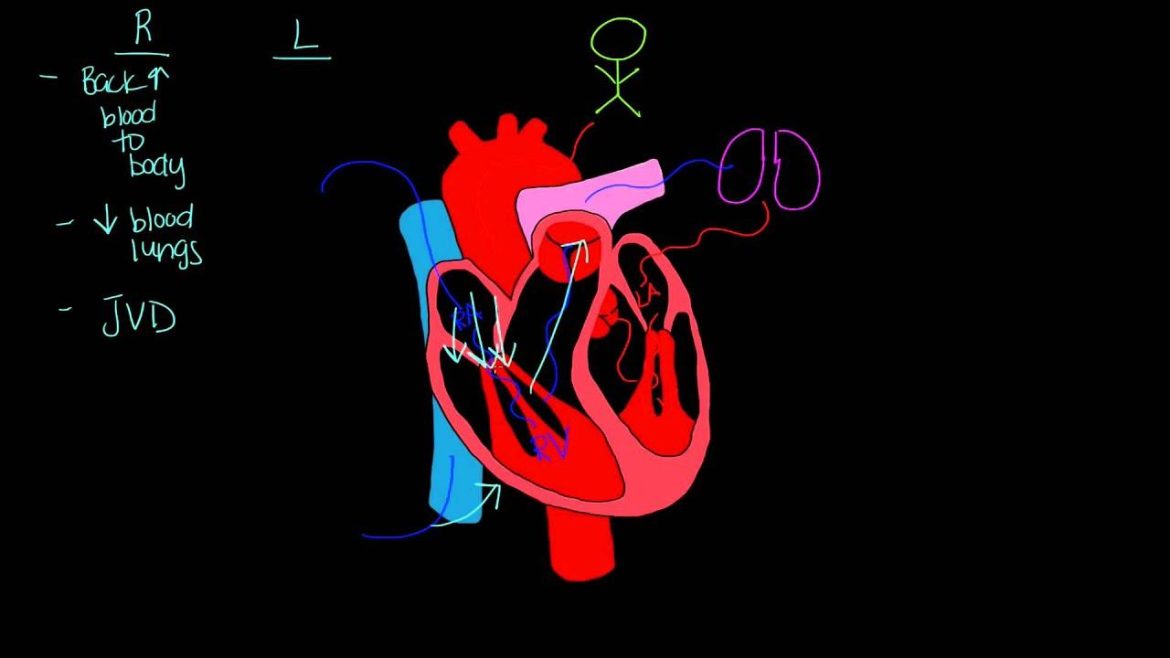
To grasp the backward effects of left-sided heart failure, it’s essential to review the normal anatomy and function of the heart’s left ventricle. The left ventricle receives oxygen-rich blood from the lungs via the pulmonary veins and pumps it into the systemic circulation through the aorta. In LHF, impaired ventricular function compromises this process, leading to inadequate blood flow to the body’s organs and tissues.
What Are The Backward Effects of Left-Sided Heart Failure
1. Backward Effects on Pulmonary Circulation
The primary backward effect of left-sided heart failure involves the pulmonary circulation, where blood backs up into the lungs due to the left ventricle’s inability to adequately eject blood forward. This leads to:
Pulmonary Congestion and Edema: Increased pressure in the pulmonary veins causes fluid leakage into the lungs’ interstitial spaces and alveoli, resulting in pulmonary congestion and edema. Patients experience symptoms such as dyspnea (shortness of breath), orthopnea (difficulty breathing while lying down), and paroxysmal nocturnal dyspnea (sudden awakening at night due to difficulty breathing).
Pulmonary Hypertension: Chronic elevation of pressure in the pulmonary circulation, secondary to left-sided heart failure, can lead to pulmonary hypertension. This condition further exacerbates right ventricular dysfunction and increases the risk of right-sided heart failure.
2. Backward Effects on Systemic Circulation
In addition to pulmonary consequences, left-sided heart failure affects systemic circulation, leading to:
Decreased Cardiac Output: As the left ventricle fails to effectively pump blood forward, systemic perfusion is compromised, resulting in decreased cardiac output. This manifests clinically as fatigue, exercise intolerance, and poor organ perfusion.
Activation of Neurohormonal Responses: The body compensates for reduced cardiac output by activating neurohormonal mechanisms, such as the sympathetic nervous system and the renin-angiotensin-aldosterone system (RAAS). These responses aim to maintain blood pressure and perfusion but can contribute to further cardiac remodeling and dysfunction over time.
Systemic Congestion: In severe cases of left-sided heart failure, inadequate forward flow of blood can cause fluid retention and systemic congestion. This leads to peripheral edema, ascites (abdominal fluid accumulation), and hepatomegaly (enlargement of the liver).
Clinical Manifestations And Diagnosis
The clinical presentation of left-sided heart failure varies depending on its severity and chronicity. Diagnostic evaluation typically includes:
Physical Examination: Assessing for signs such as elevated jugular venous pressure, pulmonary crackles, and peripheral edema.
Imaging Studies: Chest X-ray and echocardiography to evaluate cardiac structure and function.
Laboratory Tests: Including brain natriuretic peptide (BNP) levels, which can aid in diagnosing and assessing the severity of heart failure.
Management And Treatment Strategies
The management of left-sided heart failure aims to alleviate symptoms, improve quality of life, and reduce morbidity and mortality.
Treatment strategies include:
Pharmacological Therapy: Medications such as diuretics, ACE inhibitors, beta-blockers, and aldosterone antagonists are commonly prescribed to reduce symptoms, prevent disease progression, and manage fluid retention.
Lifestyle Modifications: Including dietary changes (low sodium diet), regular exercise within functional capacity, smoking cessation, and weight management.
Device Therapy: In advanced cases, devices like implantable cardioverter-defibrillators (ICDs) or cardiac resynchronization therapy (CRT) devices may be indicated to improve cardiac function and outcomes.
Surgical Interventions: Valve repair or replacement surgery may be necessary in cases of valvular heart disease contributing to left-sided heart failure.
Prognosis And Complications
The prognosis of left-sided heart failure varies depending on the underlying etiology, severity of symptoms, and response to treatment. Complications may include:
Acute Decompensated Heart Failure: Sudden worsening of symptoms requiring hospitalization and intensive management.
Arrhythmias: Increased risk of atrial fibrillation and ventricular arrhythmias.
Cardiogenic Shock: Severe reduction in cardiac output leading to multiorgan failure and high mortality rates if not promptly managed.
Conclusion
In conclusion, left-sided heart failure exerts significant backward effects on both pulmonary and systemic circulation, leading to clinical manifestations such as pulmonary congestion, systemic congestion, decreased cardiac output, and activation of neurohormonal responses. Early recognition, comprehensive evaluation, and timely intervention are essential in managing this chronic progressive condition effectively.