Coronary heart disease (CHD) is a significant health concern globally, characterized by the narrowing or blockage of coronary arteries. This can lead to various forms of angina, a condition marked by chest pain or discomfort due to reduced blood flow to the heart muscle. While the term “metal angina” is not commonly used in medical literature, it may refer to different types of angina related to metallic stents or other metal-related interventions in treating CHD. This article explores the types of angina associated with metal implants and their implications in coronary heart disease.
Understanding Angina And Its Types
Angina is a symptom of coronary artery disease (CAD) and is typically categorized into three main types:
Stable Angina: This type of angina occurs predictably with physical exertion or stress and usually subsides with rest or medication.
Unstable Angina: A more severe form that can occur at rest, indicating a higher risk of a heart attack. It requires immediate medical attention.
Variant (Prinzmetal) Angina: Caused by a spasm in a coronary artery, leading to temporary reduction of blood flow to the heart. It often occurs at rest and can be severe.
SEE ALSO: 5 Types of Chest Pain Related to Coronary Artery Disease
Introduction to Metal Angina
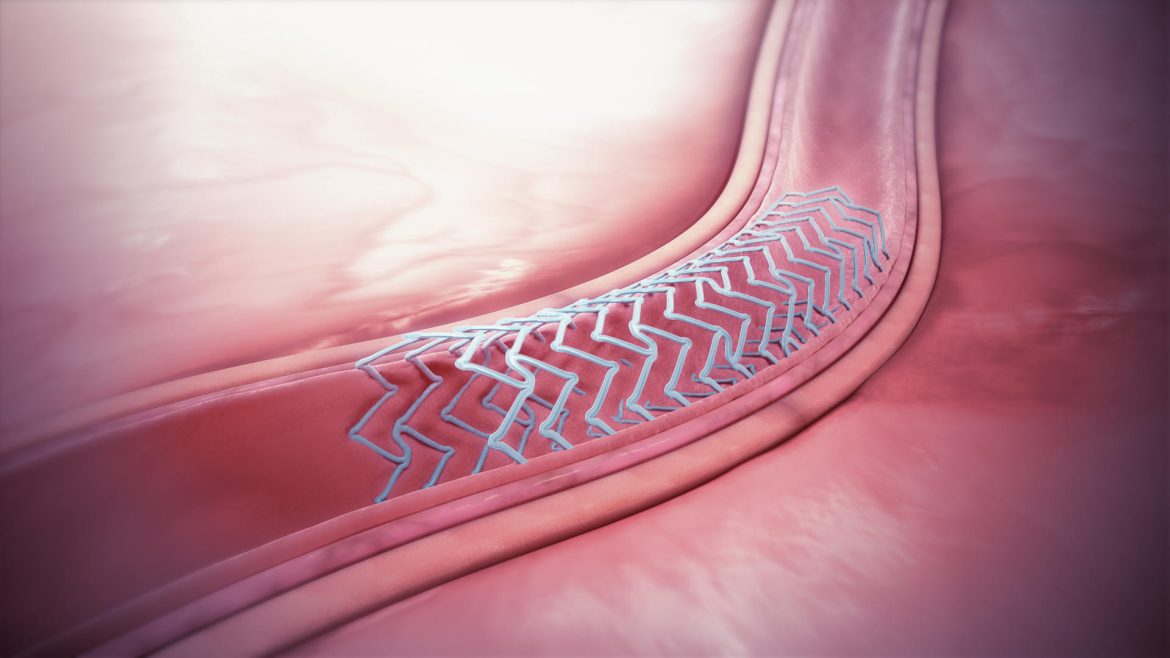
The concept of “metal angina” likely arises from complications or issues related to metal stents used in percutaneous coronary interventions (PCI). Stents are small, expandable tubes made of metal (often stainless steel or cobalt-chromium alloys) used to keep the coronary arteries open after angioplasty. While highly effective, these metal implants can sometimes lead to angina due to various factors:
- In-Stent Restenosis (ISR)
- Stent Thrombosis
- Allergic Reactions to Metal
- In-Stent Restenosis (ISR)
- Definition and Causes
In-stent restenosis refers to the re-narrowing of a previously stented coronary artery segment. It typically occurs months to years after stent placement. ISR is caused by excessive tissue growth (neointimal hyperplasia) within the stent, leading to reduced blood flow and recurrence of angina symptoms.
Risk Factors
Diabetes Mellitus: Patients with diabetes are at higher risk due to their propensity for rapid tissue growth and inflammation.
Small Vessel Size: Smaller arteries have a higher chance of re-narrowing post-stent placement.
Length and Type of Stent: Longer stents and certain types (bare-metal stents) are more prone to restenosis.
Symptoms And Diagnosis
Symptoms of ISR are similar to the original angina and may include chest pain, shortness of breath, and fatigue during physical activity. Diagnosis typically involves stress testing, angiography, or advanced imaging techniques like intravascular ultrasound (IVUS) or optical coherence tomography (OCT).
Management And Treatment
Treatment options for ISR include:
Repeat Angioplasty: Re-opening the narrowed segment with another balloon angioplasty.
Drug-Eluting Stents (DES): These stents release medication to inhibit tissue growth, reducing the risk of restenosis.
Atherectomy: Removal of the excess tissue growth using specialized devices.
Stent Thrombosis
Definition and Causes
Stent thrombosis is a serious, albeit rare, complication where a blood clot forms inside the stent, blocking blood flow. This can occur shortly after stent placement (acute), within the first month (subacute), or even years later (late and very late stent thrombosis).
Risk Factors
Non-compliance with Antiplatelet Therapy: Patients are prescribed dual antiplatelet therapy (DAPT) post-stent placement to prevent clots. Non-adherence increases the risk.
Complex Lesions: Stents placed in complex or multiple lesions are more prone to thrombosis.
Stent Malapposition: Improper stent placement can lead to gaps between the stent and artery wall, encouraging clot formation.
Symptoms and Diagnosis
Stent thrombosis often presents as sudden and severe chest pain, indicative of a heart attack. Emergency angiography is typically used for diagnosis.
Management and Treatment
Immediate PCI: Re-opening the blocked artery is critical and often involves repeat angioplasty or additional stenting.
Thrombolytic Therapy: Medications to dissolve the clot may be used in certain cases.
Intensive Antiplatelet Therapy: Adjustments or intensification of antiplatelet medications are often necessary.
Allergic Reactions to Metal
Definition and Causes
Although rare, some patients may develop allergic reactions to the metal components of stents, such as nickel or chromium.
These reactions can lead to localized inflammation, vessel narrowing, and angina.
Symptoms and Diagnosis
Symptoms include persistent chest pain post-stent placement, not explained by restenosis or thrombosis. Skin testing or blood tests can help diagnose metal allergies.
Management and Treatment
Medication: Anti-inflammatory drugs or corticosteroids may be used to manage symptoms.
Stent Removal or Replacement: In severe cases, the stent may need to be replaced with a different type, such as a polymer-based or bioresorbable stent.
Preventive Measures And Future Directions
Advancements in Stent Technology
To mitigate the risks associated with metal stents, newer technologies have been developed:
Drug-Eluting Stents (DES): Coated with medication to prevent neointimal hyperplasia.
Bioabsorbable Stents: Designed to dissolve over time, reducing long-term risks.
Polymer-Coated Stents: Reducing the risk of allergic reactions.
Lifestyle And Medication Compliance
Patients are advised to:
Adhere to Medication Regimens: Strict adherence to prescribed antiplatelet therapy is crucial.
Adopt Heart-Healthy Lifestyles: Including a balanced diet, regular exercise, smoking cessation, and managing underlying conditions like diabetes and hypertension.
Regular Monitoring and Follow-Up
Regular follow-up with healthcare providers, including stress tests and imaging, helps in early detection and management of complications.
Conclusion
Understanding the types of angina associated with metal stents is essential for both patients and healthcare providers. In-stent restenosis, stent thrombosis, and allergic reactions to metal are key complications that can lead to recurrent angina.
Advances in stent technology and adherence to preventive measures play a significant role in minimizing these risks and improving outcomes for patients with coronary heart disease.