Hyperlipidemia, characterized by elevated levels of lipids (fats) in the blood, is a condition that significantly impacts metabolic health. While its association with cardiovascular diseases like myocarditis is well-documented, its connection to pancreatitis might seem less intuitive but equally significant. This article delves into the intricate relationship between hyperlipidemia and pancreatitis, exploring the mechanisms, risk factors, and clinical implications of this complex interplay.
Understanding Hyperlipidemia
Hyperlipidemia refers to elevated levels of lipids in the bloodstream, particularly cholesterol and triglycerides. These lipids are essential for various physiological functions but can become problematic when their levels exceed normal ranges.
Hyperlipidemia is often categorized into different types based on the specific lipid involved and its density, such as hypercholesterolemia (elevated cholesterol) and hypertriglyceridemia (elevated triglycerides).
The Pathophysiology of Pancreatitis
Pancreatitis is characterized by inflammation of the pancreas, a vital organ involved in digestion and glucose metabolism.
Acute pancreatitis is typically triggered by factors such as gallstones, alcohol abuse, infections, or certain medications.
Chronic pancreatitis, on the other hand, often develops over time and is associated with long-term pancreatic damage and dysfunction.
SEE ALSO: Does Eating Too Many Eggs Give You High Cholesterol?
Why Does Hyperlipidemia Cause Pancreatitis?
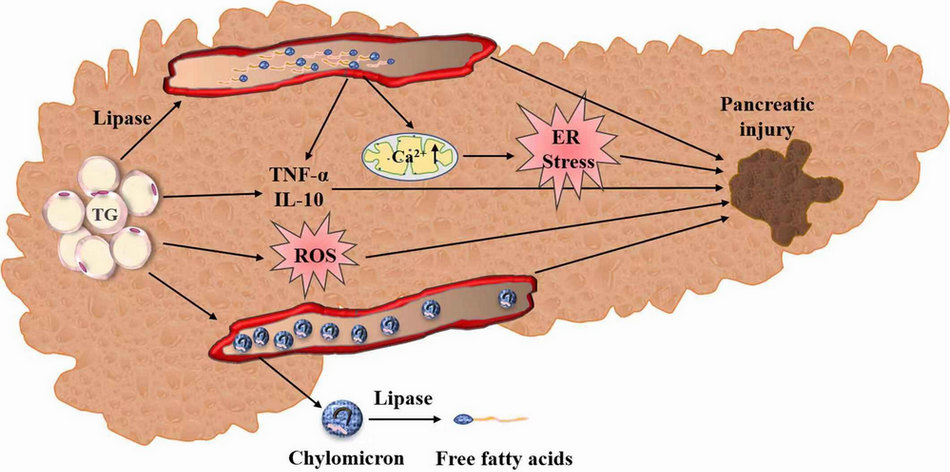
Pathogenic Mechanisms: Elevated levels of triglycerides in hyperlipidemia can lead to the accumulation of free fatty acids (FFAs) within pancreatic cells. These FFAs are toxic to pancreatic tissue, causing cellular injury and inflammation.
Moreover, hyperlipidemia can induce oxidative stress and impair mitochondrial function in pancreatic cells, further exacerbating tissue damage.
Role of Lipoproteins: Lipoproteins such as chylomicrons and very-low-density lipoproteins (VLDL) transport triglycerides in the blood. In conditions of severe hypertriglyceridemia, these lipoproteins can accumulate in the microvasculature of the pancreas, leading to ischemia (reduced blood flow) and subsequent pancreatitis.
Genetic Predispositions: Certain genetic mutations or disorders, such as familial hypertriglyceridemia or lipoprotein lipase deficiency, predispose individuals to severe hyperlipidemia. These genetic factors can significantly increase the risk of developing pancreatitis, particularly acute pancreatitis triggered by lipid-induced injury.
Clinical Implications And Management
Diagnosis Challenges: Detecting hyperlipidemia-associated pancreatitis can be challenging due to overlapping symptoms with other forms of pancreatitis. Laboratory tests measuring lipid profiles, including triglyceride levels, are crucial in identifying underlying hyperlipidemia.
Treatment Strategies: Managing hyperlipidemia involves lifestyle modifications (dietary changes, regular exercise) and pharmacological interventions (statins, fibrates) aimed at lowering lipid levels. For individuals with recurrent episodes of pancreatitis related to severe hypertriglyceridemia, specialized therapies such as plasmapheresis may be considered to rapidly reduce triglyceride levels.
Preventive Measures: Prevention strategies focus on controlling lipid levels through dietary management, avoiding alcohol consumption, and closely monitoring lipid profiles in high-risk individuals. Early intervention and adherence to lipid-lowering therapies are essential in reducing the risk of pancreatitis and its associated complications.
Conclusion
In conclusion, hyperlipidemia represents a significant risk factor for pancreatitis, contributing to both acute and chronic forms of pancreatic inflammation through various pathophysiological mechanisms. Understanding the link between hyperlipidemia and pancreatitis underscores the importance of comprehensive lipid management and early detection in clinical practice. By addressing lipid abnormalities effectively, healthcare providers can mitigate the risk of pancreatitis and improve overall patient outcomes in individuals with hyperlipidemia.
This article has explored the multifaceted relationship between hyperlipidemia and pancreatitis, shedding light on its mechanisms, clinical implications, and therapeutic considerations. As research continues to unravel the complexities of lipid metabolism and pancreatic function, ongoing advancements in diagnostic techniques and treatment modalities will further refine our approach to managing this challenging condition.
FAQs
Can Hyperlipidemia Cause Pancreatitis?
Hyperlipidemia, particularly elevated levels of triglycerides, can indeed cause pancreatitis. When triglyceride levels in the blood become excessively high (typically above 1000 mg/dL), they can lead to the development of pancreatitis. This occurs through several mechanisms:
Intracellular Lipid Deposition: Excess triglycerides can accumulate within pancreatic cells. These triglycerides are broken down into free fatty acids (FFAs) by pancreatic lipases, leading to cellular injury and inflammation.
Microvascular Damage: Lipoproteins carrying triglycerides, such as chylomicrons and very-low-density lipoproteins (VLDL), can accumulate in the microvasculature of the pancreas. This accumulation can impair blood flow (ischemia) to pancreatic tissue, triggering inflammation and pancreatitis.
Oxidative Stress: High triglyceride levels can increase oxidative stress within pancreatic cells, leading to further damage and inflammation.
Overall, severe hypertriglyceridemia is a recognized cause of acute pancreatitis and can contribute to recurrent episodes if not effectively managed.
How Does High Cholesterol Affect the Pancreas?
While hypertriglyceridemia is more directly implicated in pancreatitis, high cholesterol levels (hypercholesterolemia) can also affect the pancreas, albeit through different mechanisms:
Atherosclerosis: Elevated cholesterol levels contribute to the buildup of plaque in blood vessels (atherosclerosis), including those supplying the pancreas. This can potentially reduce blood flow to the pancreas over time, though the direct link to pancreatitis is less clear compared to triglycerides.
Indirect Effects: High cholesterol often coexists with other metabolic conditions (e.g., obesity, diabetes) that can indirectly impact pancreatic health and function. However, cholesterol itself is not typically a direct cause of pancreatitis unless severe atherosclerosis affects pancreatic blood flow.
How Does High Fat Cause Pancreatitis?
High fat intake, particularly during episodes of acute binge eating or in individuals with underlying conditions like hyperlipidemia, can trigger acute pancreatitis. The mechanism involves:
Excessive Stimulation of Pancreatic Enzymes: After consuming a large amount of fat, the pancreas releases digestive enzymes (lipases) to break down fats. In susceptible individuals, particularly those with underlying hyperlipidemia or genetic predispositions, this process can lead to an excessive release of enzymes, causing pancreatic inflammation.
Biliary Factors: High-fat diets can also exacerbate the effects of gallstones or biliary sludge, which are common causes of acute pancreatitis. Gallstones can obstruct the pancreatic duct, leading to enzyme backup and subsequent inflammation.
In summary, while hypertriglyceridemia is a direct cause of pancreatitis, high cholesterol can affect pancreatic health indirectly through vascular and metabolic pathways. High fat intake can trigger acute pancreatitis episodes, especially in individuals with underlying pancreatic vulnerabilities.