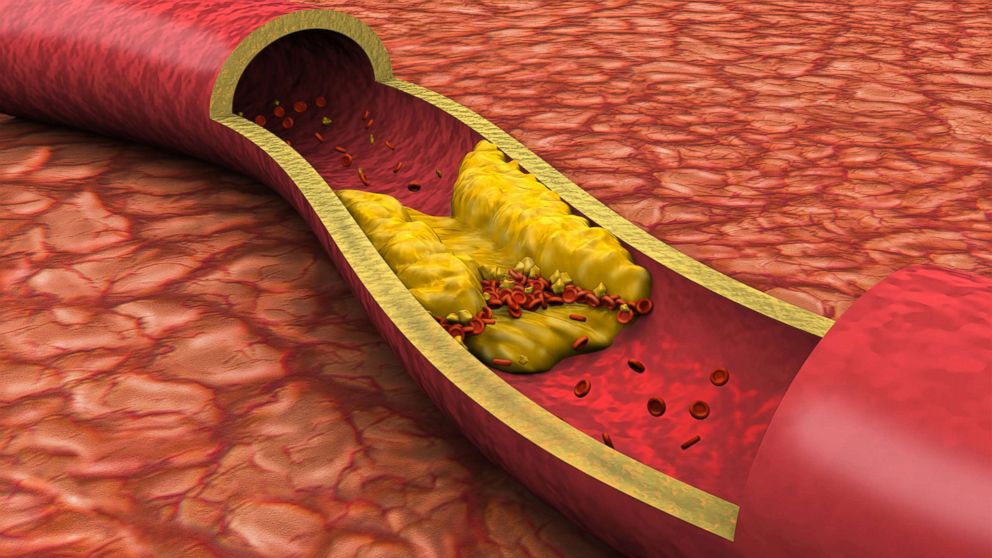
Coronary heart disease (CHD) is one of the leading causes of morbidity and mortality worldwide. It occurs when the coronary arteries, which supply blood to the heart muscle, become narrowed or blocked due to the buildup of cholesterol and other materials, forming plaque. This condition can lead to serious complications such as heart attacks, heart failure, and arrhythmias. Understanding the risks associated with coronary heart disease is crucial for prevention and management.
In this article, we will explore two significant risks of coronary heart disease: high blood pressure and high cholesterol.
1. High Blood Pressure: A Silent Risk
High blood pressure, or hypertension, is often referred to as a silent killer because it typically has no symptoms until it causes significant damage to the heart and arteries. When blood pressure is consistently high, it exerts excessive force against the walls of the arteries, causing them to become damaged and hardened. This process, known as arteriosclerosis, can lead to the narrowing of the coronary arteries, restricting blood flow to the heart muscle.
see also: 4 Warning Signs of Coronary Artery Disease
The Mechanics of Hypertension and CHD
The relationship between hypertension and CHD is well-documented. Elevated blood pressure increases the workload on the heart, causing the heart muscle to thicken and become less efficient. Over time, this can lead to left ventricular hypertrophy, a condition where the heart’s left ventricle becomes enlarged and weakened. This weakened heart muscle is less capable of pumping blood effectively, increasing the risk of heart failure.
Moreover, high blood pressure contributes to the development and progression of atherosclerosis. The constant pressure damages the endothelium, the inner lining of the arteries, making it easier for cholesterol and other substances to adhere to the artery walls. This accumulation forms plaques, which can obstruct blood flow and lead to ischemia, a condition where the heart muscle is deprived of oxygen. Ischemia can cause chest pain (angina) and, if severe, can result in a heart attack.
Epidemiological Evidence
Epidemiological studies have consistently shown a strong association between hypertension and the risk of CHD. The Framingham Heart Study, a long-term, ongoing cardiovascular cohort study, has provided extensive data on the impact of high blood pressure on heart disease. According to the study, individuals with hypertension are two to three times more likely to develop CHD compared to those with normal blood pressure levels.
Prevention and Management
Managing high blood pressure is essential for reducing the risk of CHD. Lifestyle modifications, such as maintaining a healthy diet, engaging in regular physical activity, reducing salt intake, limiting alcohol consumption, and avoiding tobacco use, can help lower blood pressure. Additionally, medications such as diuretics, ACE inhibitors, angiotensin II receptor blockers (ARBs), beta-blockers, and calcium channel blockers are commonly prescribed to control hypertension.
Regular monitoring of blood pressure is crucial for early detection and management. The American Heart Association recommends that adults have their blood pressure checked at least once every two years if their levels are within the normal range, and more frequently if they have a history of hypertension or other risk factors for CHD.
2. High Cholesterol: The Building Blocks of Plaque
High cholesterol, particularly low-density lipoprotein (LDL) cholesterol, is another major risk factor for coronary heart disease. Cholesterol is a fatty substance that is essential for building cell membranes and producing hormones. However, when there is too much LDL cholesterol in the blood, it can deposit in the walls of the arteries, leading to the formation of plaques. These plaques can narrow or block the coronary arteries, reducing blood flow to the heart.
The Role of Cholesterol in Atherosclerosis
Cholesterol is carried in the blood by lipoproteins. LDL, often referred to as “bad” cholesterol, is responsible for transporting cholesterol to the cells. When there is an excess of LDL cholesterol, it can penetrate the arterial walls and accumulate, forming fatty streaks. Over time, these fatty streaks evolve into atherosclerotic plaques. These plaques consist of cholesterol, fatty substances, cellular waste products, calcium, and fibrin (a clotting material).
As plaques grow, they cause the arterial walls to thicken and lose elasticity, a condition known as atherosclerosis. The narrowed arteries restrict blood flow, which can result in chest pain, shortness of breath, and other symptoms of CHD. If a plaque ruptures, it can trigger the formation of a blood clot, which can completely block the artery and cause a heart attack.
Genetic and Lifestyle Factors
The levels of cholesterol in the blood are influenced by both genetic and lifestyle factors. Familial hypercholesterolemia is a genetic disorder characterized by extremely high levels of LDL cholesterol, which significantly increases the risk of CHD. However, lifestyle factors such as diet, physical activity, and smoking also play a crucial role in determining cholesterol levels.
Diets high in saturated fats, trans fats, and cholesterol can raise LDL cholesterol levels. Saturated fats are found in animal products such as meat, butter, and cheese, while trans fats are present in many processed foods and baked goods. On the other hand, a diet rich in fruits, vegetables, whole grains, and healthy fats (such as those found in nuts, seeds, and fish) can help lower LDL cholesterol and increase high-density lipoprotein (HDL) cholesterol, which is known as “good” cholesterol because it helps remove cholesterol from the arteries.
The Importance of Regular Screening
Regular screening for cholesterol levels is vital for the early detection and management of hypercholesterolemia. The American Heart Association recommends that adults aged 20 and older have their cholesterol checked every four to six years, and more frequently if they have risk factors for CHD. A lipid panel test measures total cholesterol, LDL cholesterol, HDL cholesterol, and triglycerides (another type of fat in the blood).
Treatment and Management
The management of high cholesterol involves both lifestyle modifications and medication. Adopting a heart-healthy diet, engaging in regular physical activity, maintaining a healthy weight, and avoiding tobacco smoke can all help lower cholesterol levels. In addition, medications such as statins, bile acid sequestrants, cholesterol absorption inhibitors, and PCSK9 inhibitors are commonly prescribed to reduce LDL cholesterol and lower the risk of CHD.
Statins are the most widely used cholesterol-lowering drugs. They work by inhibiting an enzyme involved in the production of cholesterol in the liver, thereby reducing LDL cholesterol levels. Statins have been shown to significantly reduce the risk of heart attacks, strokes, and other cardiovascular events in individuals with high cholesterol.
Conclusion
Coronary heart disease is a major health concern that requires a comprehensive approach to prevention and management.
High blood pressure and high cholesterol are two significant risk factors that contribute to the development and progression of CHD. By understanding the mechanisms through which these risk factors affect the heart and taking proactive steps to manage them, individuals can significantly reduce their risk of developing coronary heart disease and its associated complications.