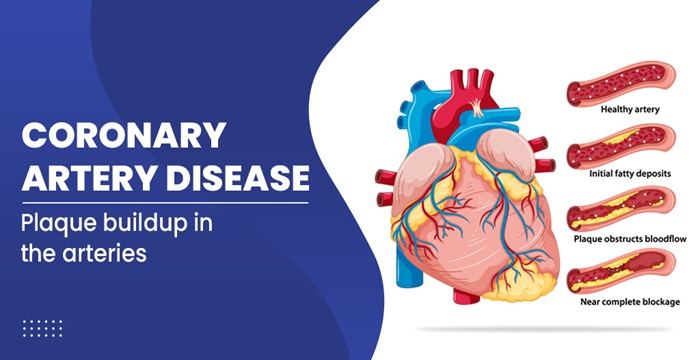
Coronary artery disease (CAD) is a condition characterized by the narrowing or blockage of the coronary arteries due to the buildup of plaque, which consists of fat, cholesterol, and other substances. This condition can lead to reduced blood flow to the heart, causing symptoms such as chest pain (angina), shortness of breath, and even heart attacks. When diagnosed in its mild form, coronary artery disease can often be managed with lifestyle changes and medical treatments aimed at reducing symptoms and preventing the progression of the disease. In this article, we will explore five effective treatments for mild coronary artery disease.
1. Lifestyle Modifications
Adopting a Heart-Healthy Diet
A heart-healthy diet is one of the most effective ways to manage mild coronary artery disease. This diet emphasizes the consumption of fruits, vegetables, whole grains, lean proteins, and healthy fats. Key components of a heart-healthy diet include:
Reducing Saturated and Trans Fats: These fats can increase cholesterol levels and contribute to plaque buildup. Opt for healthier fats such as those found in olive oil, avocados, and nuts.
Limiting Sodium Intake: Excessive sodium can raise blood pressure, which can exacerbate coronary artery disease. Aim for a daily sodium intake of less than 2,300 milligrams.
Increasing Fiber Intake: Foods high in fiber, such as whole grains, fruits, and vegetables, can help lower cholesterol levels and improve heart health.
Choosing Lean Proteins: Opt for lean meats, poultry, fish, beans, and legumes. Fatty fish like salmon and mackerel are particularly beneficial due to their omega-3 fatty acids, which have heart-protective properties.
SEE ALSO: 4 Warning Signs of Coronary Artery Disease
Engaging in Regular Physical Activity
Regular physical activity is crucial for maintaining cardiovascular health and managing mild coronary artery disease.
Exercise helps improve blood circulation, reduce blood pressure, and maintain a healthy weight. Recommended activities include:
Aerobic Exercise: Activities such as walking, jogging, cycling, and swimming can help strengthen the heart and improve overall cardiovascular fitness. Aim for at least 150 minutes of moderate-intensity aerobic exercise per week.
Strength Training: Incorporating strength training exercises two or more days a week can help build muscle, improve metabolism, and support weight management.
Flexibility and Balance Exercises: Yoga and stretching exercises can enhance flexibility, reduce stress, and improve overall well-being.
Quitting Smoking and Limiting Alcohol Consumption
Smoking is a major risk factor for coronary artery disease, as it damages the blood vessels and promotes plaque buildup.
Quitting smoking is essential for improving heart health and preventing the progression of CAD. Additionally, excessive alcohol consumption can contribute to high blood pressure and other cardiovascular issues. It is recommended to limit alcohol intake to moderate levels, which is defined as up to one drink per day for women and up to two drinks per day for men.
2. Medications
Antiplatelet Agents
Antiplatelet medications, such as aspirin and clopidogrel, are commonly prescribed to prevent blood clots from forming in the coronary arteries. These medications work by inhibiting the aggregation of platelets, which are blood cells that play a key role in clot formation. By reducing the risk of clot formation, antiplatelet agents help improve blood flow to the heart and reduce the risk of heart attacks.
Statins
Statins are a class of medications that lower cholesterol levels by inhibiting the enzyme HMG-CoA reductase, which is involved in cholesterol production in the liver. By reducing cholesterol levels, statins help prevent the buildup of plaque in the coronary arteries.
Commonly prescribed statins include atorvastatin, simvastatin, and rosuvastatin. In addition to lowering cholesterol, statins also have anti-inflammatory properties that can benefit heart health.
Beta-Blockers
Beta-blockers are medications that reduce the heart’s workload by slowing the heart rate and decreasing the force of heart contractions.
This helps lower blood pressure and reduce the oxygen demand of the heart. Beta-blockers, such as metoprolol and atenolol, are often prescribed to manage symptoms of angina and improve overall cardiovascular function.
ACE Inhibitors and ARBs
Angiotensin-converting enzyme (ACE) inhibitors and angiotensin II receptor blockers (ARBs) are medications that help relax blood vessels and reduce blood pressure. ACE inhibitors, such as lisinopril and enalapril, block the production of angiotensin II, a hormone that constricts blood vessels. ARBs, such as losartan and valsartan, block the action of angiotensin II. By reducing blood pressure, these medications help improve blood flow to the heart and reduce the risk of further coronary artery disease progression.
Nitrates
Nitrates, such as nitroglycerin, are medications that help widen blood vessels and improve blood flow to the heart. They are often used to relieve chest pain (angina) by reducing the heart’s oxygen demand and increasing the supply of oxygen-rich blood to the heart muscle.
Nitrates can be taken as needed to manage angina symptoms or used regularly to prevent angina attacks.
3. Percutaneous Coronary Intervention (PCI)
Percutaneous coronary intervention (PCI), also known as angioplasty, is a minimally invasive procedure used to treat narrowed or blocked coronary arteries. During PCI, a catheter with a balloon at its tip is inserted into the narrowed artery.
The balloon is then inflated to widen the artery and improve blood flow. In many cases, a stent (a small mesh tube) is placed in the artery to keep it open and prevent re-narrowing.
Types of Stents
Bare-Metal Stents (BMS): These stents are made of metal and provide structural support to the artery. However, there is a risk of the artery re-narrowing (restenosis) over time.
Drug-Eluting Stents (DES): These stents are coated with medication that helps prevent restenosis by inhibiting the growth of scar tissue within the artery. Drug-eluting stents have been shown to reduce the risk of restenosis compared to bare-metal stents.
Benefits of PCI
PCI is effective in relieving symptoms of angina and improving blood flow to the heart. It is typically recommended for patients with significant narrowing or blockages in the coronary arteries that are not adequately managed with medications and lifestyle changes. PCI is less invasive than coronary artery bypass surgery and offers a shorter recovery time.
4. Cardiac Rehabilitation
Cardiac rehabilitation is a comprehensive program designed to improve cardiovascular health and quality of life for individuals with coronary artery disease. The program typically includes supervised exercise training, education on heart-healthy living, and counseling to reduce stress and improve mental well-being.
Components of Cardiac Rehabilitation
Exercise Training: Supervised exercise sessions tailored to the individual’s fitness level and medical condition. Exercise helps improve cardiovascular fitness, reduce symptoms, and enhance overall well-being.
Education and Counseling: Educational sessions on heart-healthy lifestyle choices, including diet, exercise, smoking cessation, and stress management. Counseling may also address psychological aspects such as anxiety and depression.
Risk Factor Management: Ongoing monitoring and management of risk factors such as high blood pressure, high cholesterol, diabetes, and obesity. This may involve adjustments to medications and lifestyle recommendations.
Benefits of Cardiac Rehabilitation
Cardiac rehabilitation has been shown to reduce the risk of future cardiac events, improve physical fitness, enhance quality of life, and promote long-term adherence to heart-healthy behaviors. It is recommended for individuals recovering from a heart attack, angioplasty, or heart surgery, as well as those with stable angina or other forms of coronary artery disease.
5. Stress Management And Mental Health Support
Chronic stress and poor mental health can negatively impact cardiovascular health and contribute to the progression of coronary artery disease. Stress management and mental health support are important components of a comprehensive treatment plan for mild CAD.
Stress Reduction Techniques
Mindfulness and Meditation: Practices such as mindfulness meditation, deep breathing exercises, and progressive muscle relaxation can help reduce stress and promote relaxation.
Physical Activity: Regular exercise is an effective way to reduce stress and improve mood. Activities such as yoga, tai chi, and walking in nature can be particularly beneficial.
Healthy Sleep: Prioritizing good sleep hygiene and ensuring adequate rest can help reduce stress and improve overall well-being.
Mental Health Support
Counseling and Therapy: Speaking with a mental health professional can help individuals address stress, anxiety, and depression. Cognitive-behavioral therapy (CBT) is particularly effective in managing anxiety and depression associated with heart disease.
Incorporating stress reduction techniques into daily routines can have a positive impact on heart health. Finding activities that bring joy and relaxation, such as hobbies, spending time with loved ones, and practicing gratitude, can help reduce stress and improve mental well-being.
Conclusion
Managing mild coronary artery disease involves a multifaceted approach that includes lifestyle modifications, medications, medical procedures, cardiac rehabilitation, and stress management. By adopting a heart-healthy diet, engaging in regular physical activity, quitting smoking, and limiting alcohol consumption, individuals can significantly reduce their risk of disease progression.