Hyperlipidemia, characterized by elevated levels of lipids in the blood, is a significant risk factor for cardiovascular diseases, including coronary artery disease, stroke, and peripheral arterial disease. The condition is marked by high levels of cholesterol and triglycerides, substances essential for normal bodily functions but harmful in excessive amounts.
Understanding which body system is responsible for hyperlipidemia involves delving into the complex interplay of organs and processes that regulate lipid metabolism.
Which Body System Is Responsible for Hyperlipidemia?
1. The Digestive System
The digestive system plays a crucial role in the initial stages of lipid metabolism. Dietary fats are broken down in the digestive tract through the action of bile acids and digestive enzymes. These fats are then absorbed by the intestinal lining and converted into chylomicrons, lipoprotein particles that transport dietary lipids from the intestines to other parts of the body via the lymphatic system.
The liver, a key organ in the digestive system, is responsible for producing bile acids essential for lipid digestion.
Additionally, the liver processes chylomicrons and releases very low-density lipoproteins (VLDL) into the bloodstream. VLDL particles transport triglycerides and cholesterol to tissues throughout the body.
SEE ALSO: 4 Causes of Simple Hypercholesterolemia
The Central Role of the Liver
The liver is central to lipid metabolism and, consequently, hyperlipidemia. It regulates the synthesis, storage, and release of lipids and lipoproteins. The liver produces cholesterol and triglycerides, packaging them into lipoproteins for transport in the blood. It also plays a critical role in clearing lipoproteins from the bloodstream.
Several enzymes in the liver are pivotal in lipid metabolism. For instance, HMG-CoA reductase is crucial for cholesterol synthesis. When the liver’s regulatory mechanisms are disrupted, it can lead to an imbalance in lipid levels, contributing to hyperlipidemia. Factors such as genetics, diet, and lifestyle can influence liver function and lipid metabolism.
2. The Endocrine System
The endocrine system significantly influences lipid metabolism through hormones such as insulin, thyroid hormones, and corticosteroids. Insulin, produced by the pancreas, plays a vital role in regulating lipid storage and breakdown. It promotes the storage of triglycerides in adipose tissue and inhibits the breakdown of fats.
Thyroid hormones, produced by the thyroid gland, regulate basal metabolic rate and lipid metabolism. Hypothyroidism, a condition characterized by low levels of thyroid hormones, can lead to elevated cholesterol levels and contribute to hyperlipidemia. Conversely, hyperthyroidism, or excessive thyroid hormone levels, can decrease cholesterol levels.
Corticosteroids, produced by the adrenal glands, can also impact lipid metabolism. Long-term use of corticosteroid medications or conditions such as Cushing’s syndrome can lead to elevated cholesterol and triglyceride levels, contributing to hyperlipidemia.
3. The Cardiovascular System and Lipid Transport
The cardiovascular system is essential for the transport of lipids throughout the body. Lipoproteins, such as chylomicrons, VLDL, low-density lipoprotein (LDL), and high-density lipoprotein (HDL), are responsible for carrying cholesterol and triglycerides in the blood. The composition and balance of these lipoproteins determine lipid levels and influence the risk of cardiovascular diseases.
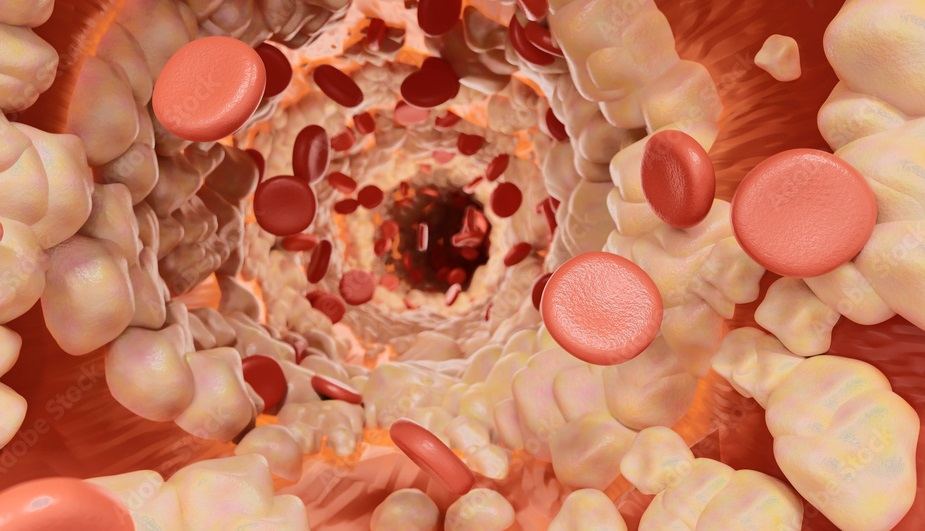
LDL, often referred to as “bad cholesterol,” transports cholesterol to tissues, where it can be deposited in the walls of arteries, leading to plaque formation and atherosclerosis. HDL, or “good cholesterol,” helps remove cholesterol from tissues and transport it back to the liver for excretion. An imbalance between LDL and HDL levels can result in hyperlipidemia and increase the risk of cardiovascular diseases.
The Genetic Component of Hyperlipidemia
Genetics play a significant role in determining an individual’s lipid levels and susceptibility to hyperlipidemia. Familial hypercholesterolemia (FH) is a genetic disorder characterized by extremely high levels of LDL cholesterol. Individuals with FH have mutations in genes responsible for LDL receptor function, leading to impaired clearance of LDL from the blood.
Genetic factors can also influence other aspects of lipid metabolism, such as triglyceride synthesis and breakdown.
Polygenic hypercholesterolemia, a condition influenced by multiple genetic variations, is another example of how genetics can contribute to hyperlipidemia. Understanding the genetic component of hyperlipidemia is crucial for identifying individuals at high risk and implementing appropriate preventive and therapeutic measures.
Diet And Lifestyle Factors
While the body’s systems play a central role in lipid metabolism, diet and lifestyle factors significantly influence the development and management of hyperlipidemia. A diet high in saturated fats, trans fats, and cholesterol can increase lipid levels and contribute to hyperlipidemia. Conversely, a diet rich in fruits, vegetables, whole grains, and healthy fats can help regulate lipid levels.
Physical activity and exercise are also crucial in managing hyperlipidemia. Regular exercise helps increase HDL levels, reduce triglycerides, and improve overall cardiovascular health. Conversely, a sedentary lifestyle can contribute to weight gain and elevated lipid levels.
Medical Management of Hyperlipidemia
The management of hyperlipidemia often involves a combination of lifestyle modifications and pharmacological interventions. Statins, a class of drugs that inhibit HMG-CoA reductase, are commonly prescribed to lower LDL cholesterol levels. Other medications, such as fibrates, niacin, and PCSK9 inhibitors, may also be used to manage lipid levels.
Lifestyle modifications, including dietary changes, increased physical activity, and weight management, are essential components of hyperlipidemia management. These measures can help reduce lipid levels, improve cardiovascular health, and reduce the risk of complications.
Conclusion
Hyperlipidemia is a multifaceted condition influenced by the complex interplay of various body systems. The digestive system, liver, endocrine system, cardiovascular system, and genetic factors all play crucial roles in lipid metabolism and the development of hyperlipidemia. Understanding the contributions of these systems is essential for effectively managing and preventing hyperlipidemia and its associated health risks.
By addressing the underlying mechanisms and implementing comprehensive lifestyle and medical interventions, individuals can better manage hyperlipidemia and reduce their risk of cardiovascular diseases. As research continues to advance our understanding of lipid metabolism, new strategies and treatments will emerge to further improve the management of hyperlipidemia and enhance overall health and well-being.